What is in this leaflet
This leaflet answers some common questions about ZYPINE and ZYPINE ODT (orally disintegrating tablets).
It does not contain all the available information. It does not take the place of talking with your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking ZYPINE against the benefits expected for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What ZYPINE is used for
ZYPINE is used to treat:
- Symptoms of schizophrenia and related psychoses
- Acute manic episodes associated with Bipolar I Disorder (as a short-term treatment) with ZYPINE alone or in combination with lithium or valproate.
- Mood stabiliser that prevents further occurrences of the disabling high and low (depressed) extremes of mood associated with Bipolar I Disorder
ZYPINE belongs to a group of medicines called antipsychotics.
This medicine helps by correcting chemical imbalances in the brain, which may cause mental illness.
Schizophrenia is a mental illness with disturbances in thinking, feelings and behaviour.
Bipolar I Disorder is a mental illness with symptoms such as feeling "high", having excessive amounts of energy, needing much less sleep than usual, talking very quickly with racing ideas and sometimes severe irritability.
ZYPINE may be used alone, or in combination with other medicines, to treat your condition.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
There is not enough information to recommend the use of this medicine for children under the age of 18 years.
This medicine is available only with a doctor's prescription.
Before you take ZYPINE
When you must not take it
Do not take ZYPINE if you have an allergy to:
- any medicine containing olanzapine
- any of the ingredients listed at the end of this leaflet.
- any other similar medicines (such as medicines of the same class or with a similar structure, as per PI).
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
Do not take this medicine if you are pregnant. It may affect your developing baby if you take it during pregnancy.
Do not breast-feed if you are taking this medicine. The active ingredient in Olanzapine passes into breast milk (if applicable) and there is a possibility that your baby may be affected.
Do not give this medicine to a child under the age of 18 years. Safety and effectiveness in children younger than 18 years have not been established.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If you take this medicine after the expiry date has passed it may not work as well.
If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor or pharmacist.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- tumour of the pituitary gland (a small gland at the base of the brain)
- disease of the blood or bone marrow with a reduced number of white or red blood cells
- disease of the blood vessels of the brain, including stroke
- prostate problems
- kidney or liver disease
- high blood sugar, diabetes or a family history of diabetes
- breast cancer or a family history of breast cancer
- paralytic ileus, a condition where the small bowel does not work properly
- epilepsy, seizures or fits
- glaucoma, a condition in which there is usually a build up of fluid in the eye
- heart disease, including irregular heart rhythm
- neuroleptic malignant syndrome, a reaction to some medicines with a sudden increase in body temperature, extremely high blood pressure and severe convulsions
- tardive dyskinesia, a reaction to some medicines with uncontrollable twitching or jerking movements of the arms and legs.
- sleep apnoea, a sleep disorder where a person has pauses in breathing or periods of shallow breathing during sleep.
Tell your doctor if you are pregnant or plan to become pregnant. Like most antipsychotic medicines, ZYPINE is not recommended for use during pregnancy. Newborn babies of mothers taking antipsychotic drugs (including ZYPINE) during the last trimester of pregnancy are at risk of experiencing extrapyramidal neurological disturbances and/or withdrawal symptoms following delivery. These may include, but are not limited to agitation, tremor, muscle stiffness or weakness, drowsiness, feeding problems, and breathing difficulty. If there is a need to consider ZYPINE during pregnancy, your doctor will discuss with you the benefits and risks of using it.
Tell your doctor if you are breastfeeding or plan to breastfeed. It is recommended that you do not breastfeed while taking ZYPINE.
Tell your doctor if you suffer from lactose intolerance (because ZYPINE tablets contain lactose).
Tell your doctor if you suffer from phenylketonuria (because ZYPINE ODT contains aspartame).
Tell your doctor if you will be in a hot environment or do a lot of vigorous exercise. ZYPINE may make you sweat less, causing your body to overheat.
Tell your doctor if you smoke. Smoking may affect ZYPINE or may affect how it works.
If you are elderly with dementiarelated psychosis, tell your doctor if you have previously had a stroke or transient ischaemic attack (ministroke) or if you have high blood pressure.
If you have not told your doctor about any of the above, tell them before you start taking ZYPINE.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and ZYPINE may interfere with each other. These include:
- medicines used to treat a fast or irregular heart beat (arrhythmia)
- medicines taken for anxiety or to help you sleep
- medicines taken for depression
- carbamazepine, a medicine used for mood stabilisation and to treat epilepsy
- other centrally acting medicines (e.g. tranquillisers or strong painkillers)
- ciprofloxacin, a medicine used to treat bacterial infections
- medicines that lower blood pressure
- medicines used for Parkinson's disease.
- medicines known to change heart's electrolyte activity or make it more likely to change.
These medicines may be affected by ZYPINE or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking ZYPINE.
How to take ZYPINE
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How much to take
Your doctor will tell you how much ZYPINE you should take. The dose your doctor will prescribe for you will usually be in the range 5 mg to 20 mg per day.
Your doctor may increase or decrease your dose in order to find the appropriate dose for your condition.
A lower starting dose may be prescribed for elderly patients over the age of 65 years.
How to take it
ZYPINE tablets should be swallowed whole with a glass of water.
ZYPINE ODT break easily, so you should handle them carefully.
Do not handle the ZYPINE ODT with wet hands as the tablets may break up.
- Hold the blister strip at the edges and separate one blister cell from the rest of the strip by gently tearing along the perforations around it.
- Carefully peel off the backing.
- Gently push the tablet out.
- Put the tablet in your mouth. It will dissolve directly in your mouth, so that it can be easily swallowed.
You can also place the tablet in a full glass or cup of water, orange juice, apple juice, milk or coffee, and stir.
Drink it straight away.
With some drinks, the mixture may change colour and possibly become cloudy.
The ZYPINE ODT should not be place in cola drinks.
When to take it
ZYPINE should be taken once a day as advised by your doctor.
Take your prescribed dose at the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
ZYPINE can be taken with or without food.
How long to take it
Continue taking your medicine for as long as your doctor tells you to.
This medicine helps to control your condition, but does not cure it. It is important to keep taking your medicine even if you feel well.
It is important that you do NOT stop taking ZYPINE unless your doctor tells you.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much ZYPINE. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much ZYPINE, the most common signs are fast heart beat, agitation/aggression, difficulty speaking, uncontrollable movements and sedation.
While you are using ZYPINE
Things you must do
It is important that you remember to take ZYPINE daily and at the dose prescribed by your doctor.
Tell all doctors, dentists and pharmacists who are treating you that you are taking ZYPINE.
While you are taking ZYPINE, tell your doctor or pharmacist before you start any new medicine.
If you become pregnant while taking ZYPINE, tell your doctor.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine. It may affect other medicines used during surgery.
If you are about to have any blood tests, tell your doctor that you are taking this medicine. It may interfere with the results of some tests.
Keep all of your doctor's appointments so that your progress can be checked.
Your doctor should monitor your weight while you are taking ZYPINE.
Patients with diabetes or who have a higher change of developing diabetes should have their blood sugar checked often.
Your doctor may request you have a blood test from time to time to monitor your cholesterol levels.
If you are over 65, your doctor may measure your blood pressure from time to time.
Tell your doctor if you are female and your monthly periods are absent for six months or more.
Talk to your doctor or mental health professional if you have thoughts or talk about death or suicide; or thoughts or talk about self-harm or doing harm to others. These may be signs of changes or worsening in your mental illness.
Things you must not do
Do not stop taking your medicine or change the dosage, even if you are feeling better, without checking with your doctor.
Do not give your medicine to anyone else, even if they have the same condition as you. Your doctor has prescribed ZYPINE for you and your condition.
Things to be careful of
Be careful driving or operating machinery until you know how ZYPINE affects you. ZYPINE may cause drowsiness in some people.
Be careful when drinking alcohol while you are taking ZYPINE. The effects of alcohol could be made worse while taking ZYPINE.
Your doctor may suggest you avoid alcohol while you are being treated with ZYPINE.
If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly. Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
If outdoors, wear protective clothing and use at least a 30+ sunscreen. ZYPINE may cause your skin to be much more sensitive to sunlight than it is normally.
Exposure to sunlight may cause a skin rash, itching, redness, or severe sunburn.
If your skin does appear to be burning, tell your doctor.
Make sure you keep cool in hot weather and keep warm in cool weather. ZYPINE may affect the way your body reacts to temperature changes. Antipsychotics have the potential to cause cardiac complications and sudden cardiac death.
Side effects
Tell your doctor or pharmacist as soon as possible if you experience any undesirable effect or feel unwell while you are taking ZYPINE.
This medicine helps most people with schizophrenia and related psychoses, short term treatment of acute manic episodes associated with Bipolar I Disorder and the prevention of reoccurring manic, mixed or depressive episodes in Bipolar I Disorder, but it may have unwanted side effects in some people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following list of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- drowsiness
- unusual tiredness or weakness
- fever
- restlessness or difficulty sitting still
- increased appetite, weight gain
- constipation, bloating
- dry mouth
- swelling of your hands, feet and ankles
- aching joints
- nose bleeds
- dizziness, confusion, forgetfulness
- speech disorder
- sleepwalking
- sleep eating.
Some people may feel dizzy in the early stages of treatment, especially when getting up from a lying or sitting position. This side effect usually passes after taking ZYPINE for a few days.
The above list includes the more common side effects of your medicine.
Tell your doctor as soon as possible if you notice any of the following:
- symptoms of sunburn (such as redness, itching, swelling or blistering of the skin) which occur more quickly than normal
- rash or allergic reaction
- slow heart beat
- changes in sexual functioning or sex drive in men or women
- prolonged and/or painful erection
- unusual secretion of breast milk
- breast enlargement in men or women
- symptoms of high sugar levels in the blood (including passing large amounts of urine, excessive thirst, having a dry mouth and skin and weakness). These may indicate the onset or worsening of diabetes
- reaction following abrupt discontinuation (profuse sweating, nausea or vomiting)
- absence of menstrual periods and changes in the regularity of menstrual periods
- involuntary passing of urine or difficulty in initiating urination
- unusual hair loss or thinning.
The above list includes serious side effects that may require medical attention.
Tell your doctor if your monthly periods are absent for six months or more.
The above list includes side effects that are uncommon but may require medical attention.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- sudden signs of an allergic reaction such as a skin rash, itching, shortness of breath or swelling of face, lips or tongue
- frequent infections such as fever, severe chills, sore throat or mouth ulcers
- bleeding or bruising more easily than normal
- painful swollen leg, chest pain, or shortness of breath as these can be signs of blood clots in the lungs or legs
- seizures, fits or convulsions
- yellowing of the skin and/or eyes
- nausea, vomiting, loss of appetite, generally feeling unwell, fever, itching, yellowing of the skin and/or eyes
- severe upper stomach pain often with nausea and vomiting (inflammation of the pancreas)
- worm-like movements of the tongue, or other uncontrolled movements of the tongue, mouth, cheeks, or jaw which may progress to the arms and legs
- sudden increase in body temperature, sweating, fast heart beat, muscle stiffness, high blood pressure and convulsions
- sharp chest pain, coughing of blood, or sudden shortness of breath
- pain/tenderness in the calf muscle area
- muscle pain, muscle weakness and brown urine.
- heart attack
- heart palpitations and dizziness, which may lead to collapse.
- fast breathing, shortness of breath, fever with chills, feeling tired or weak, chest pain while coughing, fast heartbeat. You may have pneumonia
- fever or swollen glands, especially if they occur together with or shortly after a skin rash.
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation.
All of these side effects are very rare.
The following additional side effects may occur in some groups of people taking ZYPINE.
Elderly patients with dementia-related psychosis
Elderly patients with dementia-related psychosis may notice the following side effects:
- unusual manner of walking
- falls
- pneumonia
- involuntary passing of urine
- stroke
- transient ischemic attack – symptoms maybe, but not limited to, paralysis in face, arm or leg.
Parkinson's disease psychosis
Some patients with Parkinson's disease may hallucinate (see, feel or hear things that are not there) or develop worsening symptoms of Parkinson's disease.
ZYPINE in combination with lithium or valproate
Patients with bipolar mania taking ZYPINE in combination with lithium or valproate may notice the following additional side effects:
- tremors
- speech disorder.
Tell your doctor if you notice anything unusual or if you are concerned about any aspect of your health, even if you think the problems are not connected with this medicine and are not referred to in this leaflet.
Also, some side effects, such as changes to liver function, blood cell counts, cholesterol, triglycerides, glucose and glycosuria can occur. These can only be found when your doctor does tests from time to time to check your progress.
Do not be alarmed by the above list of side effects. You may not experience any of them.
Other side effects not listed above may also occur in some patients.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
After using ZYPINE
Storage
Keep your tablets in the blister pack until it is time to take them.
Keep your tablets in a cool dry place where the temperature stays below 25°C.
Do not store ZYPINE or any other medicine in the bathroom or near a sink.
Do not leave it on a window sill or in the car.
Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
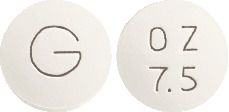
ZYPINE tablets are available in the following strengths:
2.5mg - approximately 7.0 mm normal convex, white film coated tablets debossed "OZ" over "2.5" on one side and "G" on the other side.
5mg - approximately 8.0 mm normal convex, white film coated tablets debossed "OZ" over "5" on one side and "G" on the other side.
7.5mg - approximately 9.0 mm normal convex, white film coated tablets debossed "OZ" over "7.5" on one side and "G" on the other side.
10mg - approximately 10.2 mm normal convex, white film coated tablets debossed "OZ" over "10" on one side and "G" on the other side.
Each blister pack contains 28 tablets.
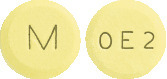
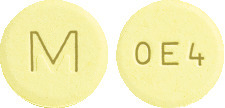
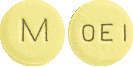
ZYPINE ODT are available in the following strengths:
5 mg - Light yellow to yellow coloured, plain to mottled, round, flat faced, beveled edged tablets debossed with "M" on one side and "OE1" on other side.
10 mg - Light yellow to yellow coloured, plain to mottled, round, flat faced, beveled edged tablets debossed with "M" on one side and "OE2" on other side.
15 mg - Light yellow to yellow coloured, plain to mottled, round, flat faced, beveled edged tablets debossed with "M" on one side and "OE3" on other side.
20 mg - Light yellow to yellow coloured, plain to mottled, round, flat faced, beveled edged tablets debossed with "M" on one side and "OE4" on other side.
Each blister pack contains 28 orally disintegrating tablets.
Ingredients
ZYPINE tablets:
- Each ZYPINE 2.5 mg tablet contains 2.5 mg of olanzapine.
- Each ZYPINE 5 mg tablet contains 5 mg of olanzapine.
- Each ZYPINE 7.5 mg tablet contains 7.5 mg of olanzapine.
- Each ZYPINE 10 mg tablet contains 10 mg of olanzapine.
The tablets also contain the following inactive ingredients:
- lactose monohydrate
- maize starch
- pregelatinised maize starch
- crospovidone
- magnesium stearate
- OPADRY AMB OY-B-28920 (ARTG PI No: 10274)
ZYPINE contains sugars as lactose and sulfites.
ZYPINE ODT:
- Each ZYPINE ODT 5 mg orally disintegrating tablet contains 5 mg of olanzapine.
- Each ZYPINE ODT 10 mg orally disintegrating tablet contains 10 mg of olanzapine.
- Each ZYPINE ODT 15 mg orally disintegrating tablet contains 15 mg of olanzapine.
- Each ZYPINE ODT 20 mg orally disintegrating tablet contains 20 mg of olanzapine.
The ZYPINE ODT orally disintegrating tablets also contain the following inactive ingredients:
- mannitol
- microcrystalline cellulose
- guar gum
- crospovidone
- magnesium stearate
- colloidal anhydrous silica
- aspartame
- sodium lauryl sulfate
ZYPINE ODT contains aspartame,phenylalanine, sulfites and glutenfrom wheat.
Supplier
ZYPINE is supplied by:
Alphapharm Pty Ltd trading as Viatris
Level 1, 30 The Bond
30-34 Hickson Road
Millers Point NSW 2000
www.viatris.com.au
Phone: 1800 274 276
This leaflet was prepared in September 2023.
Australian registration numbers:
ZYPINE tablets:
ZYPINE 2.5 mg blister pack
- AUST R 154620
ZYPINE 5 mg blister pack
- AUST R 154624
ZYPINE 7.5 mg blister pack
- AUST R 154621
ZYPINE 10 mg blister pack
- AUST R 154617
ZYPINE ODT:
ZYPINE ODT 5 mg blister pack
- AUST R 175773
ZYPINE ODT 10 mg blister pack
- AUST R 175775
ZYPINE ODT 15 mg blister pack
- AUST R 189670
ZYPINE ODT 20 mg blister pack
- AUST R 189673
ZYPINE is a Viatris company trade mark
ZYPINE_ZYPINEODT_cmi\Sep23/00
Published by MIMS October 2023





 Molecular formula: C17H20N4S. Molecular weight: 312.44.
Molecular formula: C17H20N4S. Molecular weight: 312.44.