What is in this leaflet
This leaflet answers some common questions about this medicine. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What this medicine is used for
APO-FLECAINIDE is used to treat a heart condition called arrhythmia.
Arrhythmia is an irregular or abnormal heart beat. The active ingredient flecainide acetate belongs to a group of drugs called antiarrhythmic medicines which slow down the impulses that cause the heart to beat in an irregular or abnormal way.
Your doctor may have prescribed this medicine for another purpose.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
APO-FLECAINIDE is available only with a doctor's prescription.
Before you use/are given this medicine
When you must not take it
Do not take this medicine if you have an allergy to:
- flecainide acetate
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
Do not give this medicine to children.
Do not take this medicine if you have severe heart, liver or kidney disease unless your doctor says it is suitable for you
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following conditions:
- you have used this medicine before and if you had any problems you think were caused by it
- you have or have had any kidney, liver or heart problems
Tell your doctor if you are pregnant or plan to become pregnant or are breastfeeding. Your doctor can discuss with you the risks and benefits involved.
If you have not told your doctor about any of the above, tell them before you start taking this medicine.
Do not use or have this medicine unless your doctor says it is suitable for you.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
It is particularly important to tell your doctor or pharmacist if you are taking any medicines to:
- treat high blood pressure, angina or other heart conditions, for example digoxin, propranolol, atenolol, labetalol, alprenolol, pindolol, metoprolol, timolol, oxprenolol, sotalol, disopyramide, verapamil, amiodarone, diltiazem or nifedipine
- treat stomach ulcers, for example cimetidine
These medicines may be affected by this medicine or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist may have more information on medicines to be careful of or avoid while taking or being given this medicine.
How to use this medicine
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How much to take
In adults the usual starting dose of this medicine is 50 to 100 mg every twelve hours. Your doctor may gradually increase this dose. The usual maximum dose is 300 mg a day. However, some patients may need up to 400 mg a day.
It is very important to follow your doctor's instructions exactly. Never change the dose yourself. Do not stop taking this medicine unless your doctor tells you to. Stopping this medicine suddenly may make your condition worse.
How to take it
Swallow your tablets with plenty of water. You can take the tablets before or after meals.
Your doctor may vary the dose to suit your condition.
This medicine is not recommended for use in children.
If you forget to take it
If it is almost time to take your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Never take a double dose to make up for a dose you have missed. If you miss two or more doses, please talk to your doctor.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much of this medicine. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Keep the telephone numbers of these places/services handy.
If anyone else takes some of your medicine, they should go to a hospital immediately.
While you are taking this medicine
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking this medicine.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine. It may affect other medicines used during surgery.
If you become pregnant or start to breastfeed while taking this medicine, tell your doctor immediately.
Things you must not do
Do not take this medicine to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
Things to be careful of
If you feel dizzy for any reason do not drive or operate machinery.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking this medicine.
This medicine helps most people with arrhythmia, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Tell your doctor as soon as possible if you notice any of the following:
- irregular or rapid heartbeat;
- dizziness - usually this is a minor and a temporary effect which goes away. If dizziness is severe, do not stop taking APO-FLECAINIDE but see your doctor or pharmacist
- blurred eyesight, double vision, cannot stand bright lights
- nausea
- difficulty in breathing
- tiredness
- headache, chest pain
If you experience any of these effects and find them troublesome, or if you experience any unwanted effects that are not listed here, contact your doctor or pharmacist immediately.
Storage and Disposal
Storage
Keep your tablets in the pack until it is time to take them. If you take the tablets out of the pack they may not keep well.
Keep your medicine in a cool dry place where the temperature stays below 25°C.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
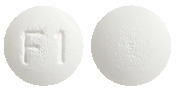
50 mg Tablets: White to off white, circular, biconvex, tablets debossed with F1 on one side and plain on other side with an approximate diameter of 6.5 mm. AUST R 289980.
100 mg Tablets: White to off white, circular, biconvex, tablets debossed with F & 2 separated by scoreline on one side and plain on other side with an approximate diameter of 8.8 mm. AUST R 289979.
Available in blister packs of 20, 30, 40, 50 and 60 tablets.
Not all packs are available.
Ingredients
APO-FLECAINIDE 50 mg tablets contain 50 mg of the active ingredient flecainide acetate.
APO-FLECAINIDE 100 mg tablets contain 100 mg of the active ingredient flecainide acetate.
This medicine also contains the following:
- silicified microcrystalline cellulose
- croscarmellose sodium
- maize starch
- magnesium stearate
Supplier
This medicine is supplied in Australia by:
Apotex Pty Ltd
16 Giffnock Avenue
Macquarie Park NSW 2113
Tel: (02) 8877 8333
Web: www1.apotex.com/au
This leaflet was last updated in September 2020.
Published by MIMS November 2020

 Molecular formula: C17H20F6N2O3.C2H4O2.
Molecular formula: C17H20F6N2O3.C2H4O2.