In October 2016 NPS MedicineWise launched the program Ankle and knee injuries: your imaging choices. This was the first therapeutic program that incorporated Choosing Wisely recommendations. The goal of the program was to reinforce the diagnostic accuracy of GPs’ clinical history-taking and physical examination skills when managing people with acute ankle and knee injuries in primary care.
In May 2017, 1200 GPs who participated in a one-to-one or group-based educational visit for this program were invited to complete a retrospective pre-test (RPT) paper questionnaire to identify trends in GP knowledge, awareness and practice in the area of diagnosis and management of acute ankle and knee injuries. 800 GPs who had not participated in the program were also asked to complete a questionnaire, as a control group for comparison. The response rate for both surveys was 20%.
NPS MedicineWise would like to thank participating GPs for taking the time to complete our surveys.
About the respondents
GPs from all states and territories completed the survey. There were differences between the participant and control groups by location, with most participating GPs in Victoria (35%) and most control GPs in NSW (37%). 35% of participant GPs and 27% of control GPs had practiced for less than 10 years, and 18% of participant GPs and 24% of control GPs had practiced for between 11 and 20 years.
The majority of GP respondents indicated that they see between one and 10 patients per month with acute ankle or knee injuries (75% of participant GPs and 79% of control GPs).
Key evaluation findings
A total of 8,786 unique health professionals participated in NPS MedicineWise ankle and knee program activities, including 7,457 GPs. The program resulted in changes to GP knowledge, confidence and practice in the diagnosis and management of acute ankle and knee injuries. GPs who took part in an educational visit were more likely to:
- apply the Ottawa Ankle and Knee Rules
- know when an X-ray is typically indicated for an acute ankle or knee injury
- know that history and physical examination can be as good as magnetic resonance imaging (MRI) for certain injuries
- be more confident communicating to patients that imaging will not change management
- be more confident using physical examination to diagnose the cause of acute knee and ankle pain as a result of injury.
GP knowledge
GP respondents who completed the RPT or control surveys were asked to identify their levels of agreement or disagreement with a number of statements about the use of X-ray, ultrasound and MRI for ankle and knee injuries.
Table 1 shows the knowledge statements and the percentages of GPs who reported the desired response both before and after participating in a visit from an NPS MedicineWise Clinical Services Specialist, as well as the desired response percentages of the control group.
Table 1: GP response to knowledge statements
| Statements | Participant responses before visit % (n) |
Participant responses after visit % (n) |
Control % (n) |
|---|---|---|---|
| An X-ray is typically indicated for acute knee or ankle pain resulting from injury. (desired response of disagree or strongly disagree) |
58 (124) | 73 (157) | 65 (99) |
| History and physical examination can be as good as MRI for diagnosis of acute anterior cruciate ligament or meniscal tear. (desired response of agree or strongly agree) |
52 (113) | 76 (165) | 61 (93) |
| MRI should be reserved for cases with unclear diagnosis after history and physical examination and only if the results will change management. (desired response of agree or strongly agree) |
85 (183) | 96 (206) | 92 (141) |
| An ultrasound and X-ray of the ankle are a useful combination to assess acute ankle injury. (desired response of disagree or strongly disagree) |
49 (105) | 59 (127) | 57 (87) |
The proportion of participant GPs selecting the desired response increased significantly for three of the four knowledge statements (Table 1).
GP confidence
GP respondents were asked to identify their levels of agreement or disagreement with statements about their confidence in using physical examinations for diagnosis and communicating with patients. Table 2 shows the statements and the percentages of GPs who reported the desired response. Among participant GPs there was a significant increase in confidence after the educational visit. GPs who had participated in an educational visit were significantly more confident in using physical examination to diagnose the cause of acute knee pain than control GPs.
Table 2: GP response to confidence statements
| Statements | Participant responses before visit % (n) |
Participant responses after visit % (n) |
Control % (n) |
|---|---|---|---|
| I am confident using physical examination to diagnose the cause of acute knee pain. (desired response of agree or strongly agree) |
60 (131) | 77 (167) | 60 (93) |
| When I believe imaging is not clinically indicated, I am confident communicating to my patients that imaging results will not change management. (desired response of agree or strongly agree) |
73 (161) | 90 (198) | 87 (133) |
The visits were also successful in prompting an increase in GP confidence in performing physical tests to diagnose acute ankle and knee injuries.
GP awareness
Awareness of Choosing Wisely Australia was higher among GPs who participated in an educational visit (66%, n = 153) than among the control group (48%, n = 72).
The majority of participant GPs (76%) and control GPs (65%) were aware of the Choosing Wisely recommendation ‘Do not request imaging for acute ankle injury unless indicated by the Ottawa Ankle Rules’. Of those who were aware of the recommendation, 91% were aware of Choosing Wisely Australia.
GPs who participated in an educational visit were significantly more aware than control GPs, of both the Ottawa ankle rules (81% vs. 31%) and the Ottawa Knee Rules (73% vs. 52%) (see Table 3).
Table 3: GP awareness of Ottawa Ankle and Knee Rules
| Rule | Respondent type | Aware % (n) |
Not aware % (n) |
|---|---|---|---|
| Ottawa Ankle Rules | Participant | 81% (191) | 19% (44) |
| Ottawa Ankle Rules | Control | 31% (47) | 69% (107) |
| Ottawa Knee Rules | Participant | 73% (172) | 27% (63) |
| Ottawa Knee Rules | Control | 52% (80) | 48% (74) |
GP practice
After the educational visit, the proportion of participant GPs who agreed or strongly agreed that they consider the risk of radiation when deciding to send a patient for an X-ray for an acute knee or ankle injury, significantly increased from 63% to 70%.
Figure 1 shows other practice statements and the percentages of GPs who reported the desired response of ‘always’. There were significant improvements for all four statements demonstrating that GPs who participated in a visit with a Clinical Services Specialist have changed their practice in positive ways.
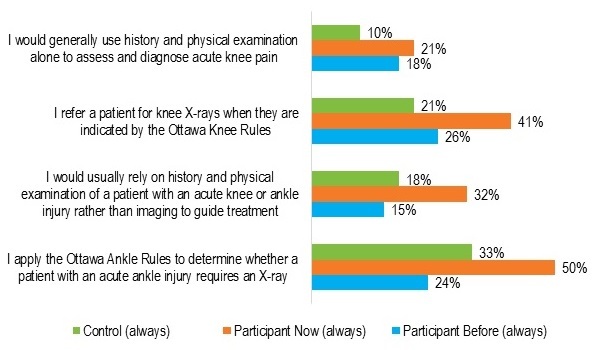
Go to an accessible version of the data for Figure 1
Figure 2 shows a number of statements with the desired response to increase practice. The majority of respondents had increased practice in all desired areas or no change was necessary. The greatest change was reported in the application of the Ottawa Ankle and Knee Rules when presented with acute ankle and knee injuries (74% increased or intended to increase).
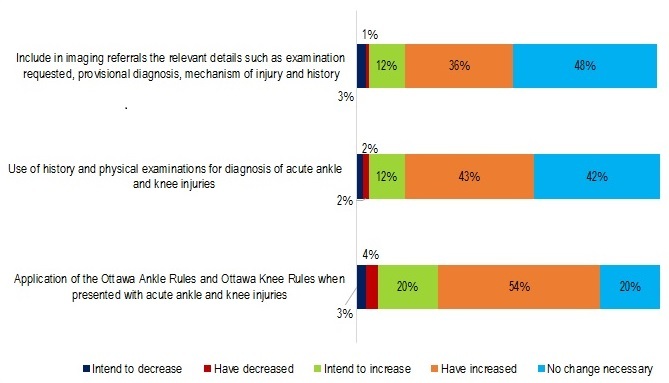
Go to an accessible version of the data for Figure 2
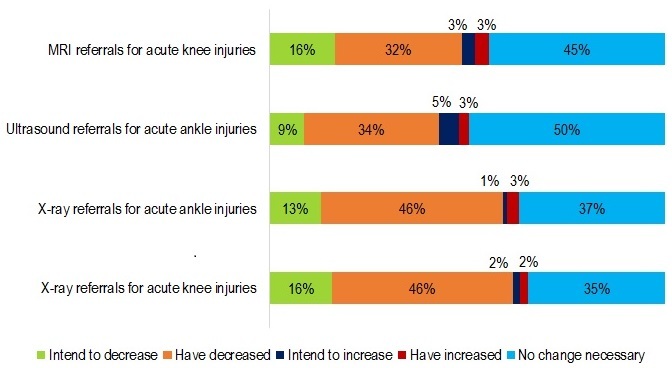
Figure 3 shows the statements with a desired response to decrease practice. The majority of respondents had decreased practice in all desired areas or no change was necessary. The greatest changes were reported in X-ray referrals for both acute ankle and acute knee injuries (59% for acute ankle injuries and 62% for acute knee injuries decreased or intended to decrease).
Summary
After the educational visit, the proportion of participant GPs who agreed or strongly agreed that they consider the risk of radiation when deciding to send a patient for an X-ray for an acute knee or ankle injury, significantly increased from 63% to 70%.
Figure 1 shows other practice statements and the percentages of GPs who reported the desired response of ‘always’. There were significant improvements for all four statements demonstrating that GPs who participated in a visit with a Clinical Services Specialist have changed their practice in positive ways.
Almost 7,500 GPs participated in the Ankle and knee injuries: your imaging choices program. Overall, GPs who participated in an educational visit for this program demonstrated significant improvements in knowledge, confidence and practice in diagnosis and of acute ankle and knee injuries.
The educational visits increased GP confidence in:
- using physical examination to diagnose the cause of acute knee pain
- communicating to patients that imaging results will not change management when imaging is not clinically indicated
- performing physical tests to diagnose acute ankle and knee injuries.
The findings showed that the visits also improved practice in the diagnosis and management of acute ankle and knee injuries with significant increases in:
- the consideration of the risk of radiation when deciding whether to send a patient for an X-ray
- the use of physical examination and history
- application of the Ottawa Ankle and Knee Rules.
They also showed a decrease in referrals for X-rays, MRIs and ultrasounds for an acute knee or ankle injury.
The survey findings will inform future programs to better serve the needs of GPs.

