In February 2017, NPS MedicineWise launched the program COPD medicines and inhalers: stepping through the options. The goal of the program was to improve quality of life for Australians with stable COPD through improved medicines management in primary care.
In 2017, 2500 GPs across Australia were invited to complete a pre- and post-survey to identify trends in GP confidence, knowledge and practice regarding the use of COPD medicines and inhalers.
A total of 443 GPs completed the pre-survey and 283 GPs completed the post-survey 9 months after participating in an educational visit.
NPS MedicineWise thanks participating GPs for taking the time to complete our surveys.
About the respondents
GPs from all states and territories completed the survey. The majority had been practicing for more than 20 years and were employed in larger practices (with three or more GPs).
GPs commonly participated in a one-to-one or group-based educational visit facilitated by an NPS MedicineWise Clinical Services Specialist.
Key evaluation findings
A total of 8311 unique GPs participated in NPS MedicineWise COPD educational visits, which exceeded expectations.
Most respondents (98%) who participated in an educational visit were ‘very satisfied’ or ‘satisfied’ with the Clinical Services Specialists, particularly their knowledge, communication style and ability to answer questions.
Following the educational visits, GPs were more likely to understand the need to:
- limit the use of inhaled corticosteroid (ICS) + long-acting beta-2 agonist (LABA) fixed-dose combinations to patients with moderate to severe COPD and frequent exacerbations
- use spirometry to confirm FEV1 < 50% predicted before stepping-up therapy to an ICS + LABA fixed-dose combination
- prescribe an ICS + LABA fixed-dose combination in patients with COPD and no asthma when FEV1 < 50% predicted and the patient has experienced two or more exacerbations in the previous year.
The GPs were also more likely to:
- use spirometry in addition to history and clinical examination to exclude asthma and asthma-COPD overlap syndrome (ACOS)
- appropriately manage COPD using a stepwise approach
- use Lung Foundation Australia’s stepwise management chart.
GP knowledge
GP respondents were asked to indicate their level of agreement with a number of knowledge statements about prescribing medicines for patients with COPD (with no overlap with asthma).
Table 1 shows the knowledge statements and the percentages of GPs who reported the desired response (‘strongly agree’ or ‘agree’) both before and after participating in a visit from an NPS MedicineWise Clinical Services Specialist.
Following the educational visits, desired responses significantly increased for each of the three knowledge statements.
Table 1: GP responses to knowledge statements
| GP responses before visit % (n) |
GP responses after visit % (n) |
Significant difference % (p-value) |
|
|---|---|---|---|
|
Use of LABA + long-acting muscarinic antagonist (LAMA) fixed-dose combination should be limited to patients with uncontrolled symptoms despite long-acting bronchodilator monotherapy |
69 (293) | 77 (216) | +8 (p = 0.011) |
| Consideration of ICS + LABA fixed-dose combination should be limited to patients with moderate to severe COPD and frequent exacerbations | 74 (318) | 85 (237) | +11 (p = 0.001) |
| Spirometry should be used before stepping-up inhaler therapy to an ICS + LABA fixed-dose combination to confirm FEV1 < 50% predicted | 50 (215) | 64 (179) | +14 (p < 0.001) |
GP respondents were also asked to indicate one situation when they would consider prescribing an ICS + LABA fixed-dose combination in patients with COPD and no asthma.
Figure 1 shows the four situations presented to GPs and percentages of GPs who selected the desired response, as per COPD guidelines, of ‘FEV1 < 50% predicted and the patient has experienced two or more exacerbations in the previous year’.
The proportion of GPs who selected the desired response significantly increased after the educational visits, from 52% to 62% (p = 0.015).
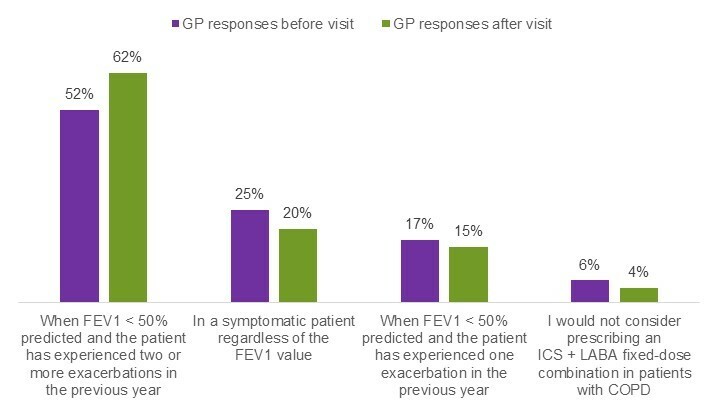
Figure 1: GP selection of a situation when they would prescribe an ICS + LABA fixed-dose combination
GP practice
Figure 2 shows the percentages of GPs who reported the desired response when they were asked the question above about controlling Marie’s symptoms. In line with COPD guidelines, the desired response was ‘step-up therapy to a combination LABA + LAMA’ inhaled medicine.
The proportion of GPs who selected the desired response significantly increased after the educational visits, from 67% to 78%.
This 11% increase met the COPD program’s objective, which pre-specified a 10% increase in the proportion of GPs who correctly diagnose and manage COPD according to Lung Foundation Australia’s stepwise criteria.
The results suggest that the educational visits effectively delivered the program’s key messages about the need to apply a stepwise approach to COPD management.
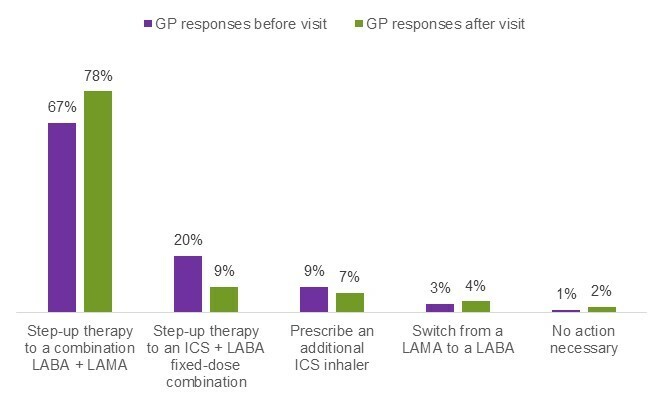
Figure 2: GP responses when asked about controlling Marie’s symptoms
Summary
The COPD educational visits attracted over 8000 GPs who were satisfied with the quality of the activity they participated in and believed it to be entirely relevant to their practice.
The Clinical Services Specialists, who delivered the program to GPs, were praised for their knowledge of the topic and their communication skills.
Overall, GP participation led to significant improvements in knowledge and practice in key areas of COPD management.
In particular, the educational visits effectively delivered key messages on correctly diagnosing and managing COPD using a stepwise approach and using spirometry.
The visits also successfully increased use of Lung Foundation Australia’s stepwise management chart.
The survey findings will inform future programs to better serve the needs of GPs.

