In October 2015, NPS MedicineWise launched a visiting program, Preventing fractures: Where to start with osteoporosis. The goal of this educational visiting program was to reduce the occurrence of fractures associated with osteoporosis in adults in the Australian population.
In April 2016, 1000 GPs who participated in a 1:1 or group-based educational visit for this program were invited to complete a retrospective pre-test (RPT) questionnaire online; 1000 GPs who had not participated in the program were also asked to complete an online survey for comparison.
The response rate for both surveys was 13%.
NPS MedicineWise would like to thank participating GPs for taking the time to complete our surveys.
About the respondents
Overall, participant and control demographics were similar. GPs from all States and Territories completed the surveys.
The majority of GPs in both groups had been practising for less than 20 years and were employed in larger practices with three or more GPs. Of the respondents, 47% of participant GPs (n = 45) and 43% of control GPs indicated that they see five or less patients with a confirmed diagnosis of osteoporosis per month.
More than half (56%) of participant GPs were involved in a 1:1 educational visit, 43% were involved in a group-based visit and 1% participated in both activities.
Key evaluation findings
The program of educational visits resulted in changes to the way GPs undertook the identification and management of osteoporosis.
GPs who took part in an educational visit were more likely to:
- consider four key osteoporosis risk factors (rheumatoid arthritis, alcohol intake ≥ 3 units per day, current smoking and parental history of fracture) in their patients
- identify optimal management for a male patient with clinical risk factors (77% vs 66%, p = 0.004)
- identify preferred practice for a female patient with minimal trauma fracture (53% vs 32%, p < 0.001)
- recognise the need to correct pre-existing hypocalcaemia before correcting osteoporosis management (92% vs 63%, p < 0.001)
- correctly identify best practice for the long-term use of bisphosphonates.
Participant GPs also reported increased confidence in assessing the risks and benefits of six commonly prescribed medicines used in osteoporosis management, particularly denosumab (42% reported an increase, p < 0.001).
In addition, a greater proportion of participant GPs reported discussing adherence-related topics with their patients after the program, especially why patients had been prescribed a particular type of medicine (88% vs 66%, p < 0.001) and explaining that medicines are a long-term investment (84% vs 51%, p < 0.001).
An educational visit did not modify prescribing considerations, consideration of oral corticosteroids as a risk factor, or practice in patient monitoring.
GP knowledge
Impact on GP knowledge was a strength of this program, with participant GPs demonstrating improved knowledge about multiple topics covered during the educational visits, especially identifying patients at risk of minimal trauma fracture.
Survey question – risk of minimal trauma fracture
Ted is a 71-year-old retired bus driver. While discussing his lifestyle, you find out that Ted smokes one pack of cigarettes per day and has 3–4 drinks in the evening to relax. Based on this information, which of the following statements do you with agree with?
For this question, participant GPs were asked to apply their knowledge of risk factors to the case of a male patient with clinical risk factors for osteoporosis. A significantly higher proportion of GPs chose the desired response for the patient’s management after taking part in an educational visit (77% vs 60%, p = 0.004; Table 1).
For this question, participant GPs were asked to apply their knowledge of risk factors to the case of a male patient with clinical risk factors for osteoporosis. A significantly higher proportion of GPs chose the desired response for the patient’s management after taking part in an educational visit (77% vs 60%, p = 0.004; Table 1).
| Treatment options | Participant response before visit % (n) | Participant response after visit % (n) |
|---|---|---|
Ted is not at risk of osteoporosis; no diagnostic investigation is required. | 15% (14) |
4% (4) |
| Ted is at risk of osteoporosis; the most important measure to determine Ted’s eligibility for PBS-subsidised osteoporosis treatment is the absolute bone mineral density. | 15% (14) | 13% (12) |
| Ted is at risk of osteoporosis; the most important measure to determine Ted’s eligibility for PBS-subsidised osteoporosis treatment is the T-score. | 60% (56) | 77% (70) |
GP practice
After participating in the program, significant improvement was demonstrated in several areas of GP practice, such as management of a patient with a minimal trauma fracture, and increased discussion of topics to encourage patient adherence to prescribed osteoporosis medications.
For this question, the preferred practice is to start osteoporosis treatment, as the patient has experienced a minimal trauma fracture. Best practice is also to use DXA for monitoring every 2 years in most cases, so the purpose of a scan at this time is to set a baseline for monitoring.
After participating in the program, a significantly increased number of participant GPs correctly identified best practice management for a female patient with minimal trauma fracture (+21%, p < 0.001; Table 2).
| Treatment options | Participant response before visit % (n) | Participant response after visit % (n) |
|---|---|---|
| Refer Margie for a DXA scan to check whether her BMD T-score warrants osteoporosis treatment | 53% (42) | 42% (38) |
| Start osteoporosis treatment with a bisphosphonate or denosumab and refer Margie for a DXA scan to establish a baseline BMD for future monitoring | 32% (28) | 53% (48) |
| Start osteoporosis treatment with a bisphosphonate or denosumab without ordering a DXA scan | 5% (4) | 1% (1) |
| The highest priority at this time is pain management; delay further investigation of osteoporosis | 5% (4) | 1% (1) |
| Refer Margie to a specialist for further investigation or treatment | 3% (2) | 2% (2) |
A greater proportion of GPs reported discussing these topics with their patients after participating in an educational visit. The areas with the greatest changes were:
- why patients had been prescribed a particular type of medicine (an increase from 66% to 88%, p < 0.001)
- signs of adverse effects for which the patient should seek immediate assistance (an increase from 59% to 86%, p<0.001)
- explain that medicines are a long-term investment (an increase from 51% to 84%, p < 0.001).
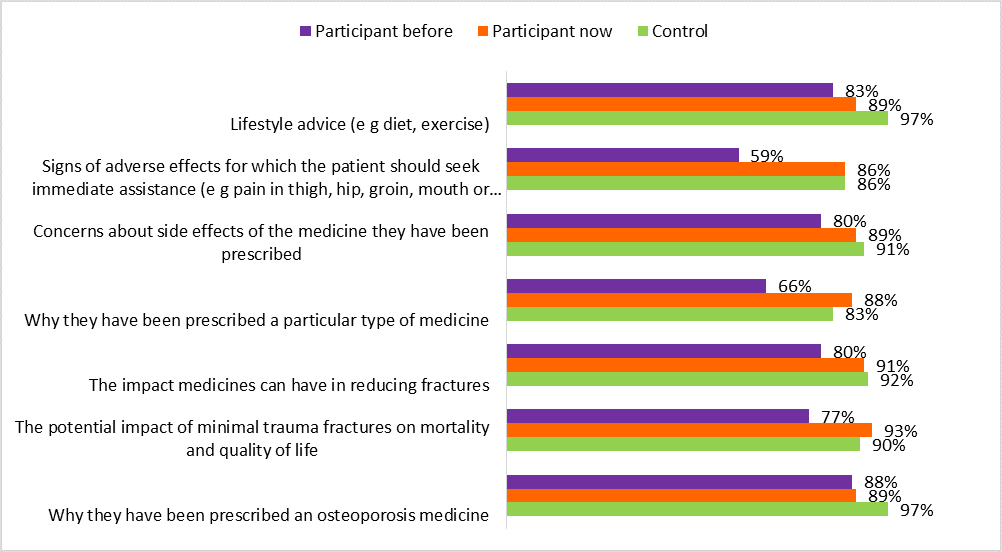
Figure 1. Percentage change in best practice management of long-term prescription of bisphosphonates after program participation
Summary
Overall, GPs who participated in an NPS MedicineWise Preventing Fractures: Where to Start with Osteoporosis activity demonstrated significant improvements in knowledge and in some areas of practice in line with program messages.
The program had positive impacts on knowledge of risk factors and identification and management of osteoporosis, levels of confidence in judging risks and benefits of medicines used, and approaches to management for at-risk patients.
Areas where changes in GP practice were not detected included assessment of oral corticosteroids as a risk factor, prescribing considerations, and patient monitoring. These results may help identify areas for focus in the design of future programs to better serve the needs of GPs.

