Non-traumatic shoulder pain in general practice: a pragmatic approach to diagnosis
Focused clinical history and physical examination is usually sufficient to diagnose non-traumatic shoulder pain in general practice, and guide management.
Key points
- Shoulder pain is a common reason for seeking health care in Australia.
- A focused clinical history and physical examination without imaging is usually sufficient to arrive at a working diagnosis and management approach for patients presenting with non-traumatic shoulder pain in general practice.
- In the absence of red flags, imaging for non-traumatic shoulder pain has limited benefits and is not likely to influence management.
- Where imaging is warranted, ensure appropriate clinical details are provided in the referral to help focus the investigation and assist the radiologist’s interpretation of the findings.
- Explain to and reassure patients that most episodes of shoulder pain have favourable outcomes.
Download and print
Shoulder pain: complex, not complicated
The shoulder is a complex structure which is highly dependent on ligaments and tendons for stability, making it prone to a range of problems.1 However, complex doesn’t necessarily mean complicated when assessing shoulder pain, and an overcomplicated approach to diagnosis is unlikely to alter early conservative management.2
Shoulder pain is a common reason for seeking medical care in Australia, with shoulder complaints accounting for 1.2% of all presentations to general practitioners in 2015-16.3
Heavy reliance on imaging in general practice may be related to low levels of practitioner confidence about making a clinical diagnosis. Patients may also expect to be told the exact cause of their pain, which could pressure GPs into ordering imaging early.4,5
Keeping it simple
A simple approach, based on history and targeted physical examination, is recommended for the assessment and management of shoulder pain. Each element of history and examination has limited reliability and validity6 but collectively they show patterns which usually lead to a working diagnosis that can inform management. Good management has the potential to improve the prognosis of shoulder pain.7
The pain history should consist of an assessment of the location, nature, severity, onset and duration of pain as well as risk factors for shoulder pain. A past history of malignancy or recent infection or trauma should alert doctors that red flags may be present.1
| History | Examination | Think of |
|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Characteristics of a clinical history are outlined in Figure 1.
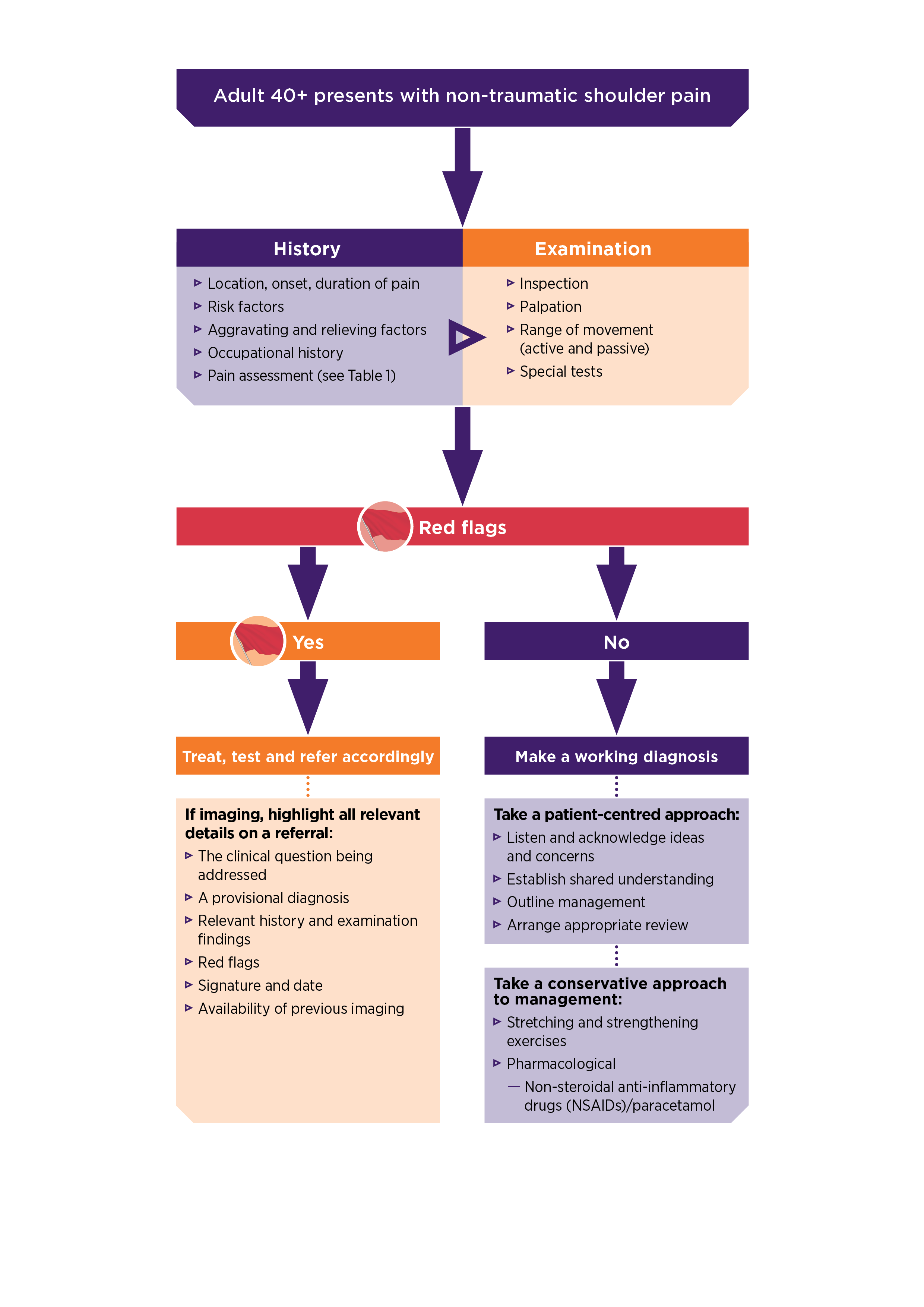
Figure 1: Characteristics of a clinical history
Read a text-only version of this graphic
A targeted physical examination
A targeted shoulder examination consists of inspection, palpation and movement testing. Comparison with the other shoulder, as appropriate, and having the shoulders adequately exposed is important.13 NPS MedicineWise has developed a clinical examination video with Dr Michael Yelland, general and musculoskeletal medicine practitioner, outlining the key aspects of each stage of the shoulder examination. This includes two special tests.
Be mindful that imaging rarely affects management
Research reports that Australian doctors rely heavily on imaging for the diagnosis and management of shoulder pain. In one Australian study, in response to a scenario of a patient with a history consistent with rotator cuff tendinopathy, 69% of GPs ordered a shoulder X-ray and 82% ordered ultrasound.14 However, the diagnostic utility of imaging is limited in non-traumatic shoulder pain and imaging is unlikely to alter management.15
Be mindful that incidental findings on imaging can lead to unnecessary further investigations and treatment
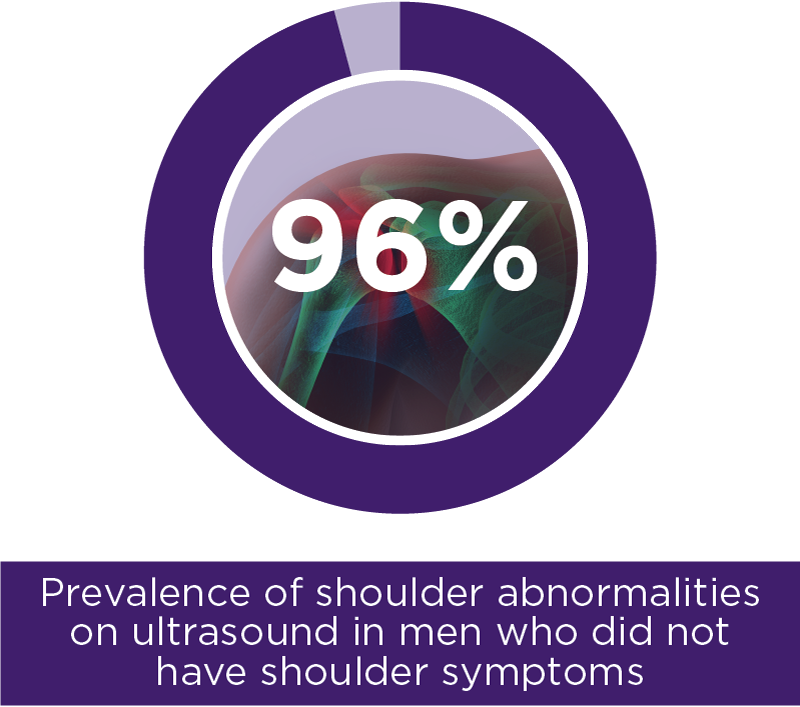
The causal link between imaging findings and shoulder symptoms is poor, with research reporting high rates of incidental findings in asymptomatic individuals.16,17 One study, which investigated ultrasound findings, reported that shoulder abnormalities were identified in 96% of men who did not have shoulder symptoms.16,18 The high prevalence of incidental finding identified in images of patients presenting with shoulder pain can complicate the interpretation of imaging results. This may lead to inappropriate treatment if the clinician associates signs and symptoms with the reported imaging findings in the absence of clinical correlation.7
Imaging modalities such as ultrasound and magnetic resonance imaging (MRI) have been reported as useful diagnostic tools in secondary care2 and may be indicated in some cases of non-traumatic shoulder pain, such as in the presence of red flags.19 In cases where imaging is warranted for red flags, X-ray is the recommended starting point due to its wide availability and accessibility.20
Definitive anatomical and pathological diagnosis of non-traumatic shoulder pain can be difficult and may not always be reliable.21-25
In recent years, approaches that reduce the emphasis on patho-anatomically based diagnostic labelling and highlight more pragmatic, functional assessment have been proposed.21,22 This approach is similar to the recommended approach to low back pain.
In this video interview, Professor Karen Ginn, musculoskeletal anatomist, physiotherapist and clinical researcher, describes her approach to assessing patients presenting with non-traumatic shoulder pain.
Make the most of your imaging request – if absolutely necessary…
The information provided on an imaging request form has a direct impact on patient care and safety. One study reported that the information on 34% of request forms contained no contributory history or clinical information for the radiologist.26 To allow the radiologist to interpret the results and provide a clinically appropriate report, it is important that key clinical details are conveyed clearly in the referral.27,28 These include:27
- the clinical question being addressed: including a clear diagnostic question will help focus the radiologist’s interpretation of results
- a provisional diagnosis: a provisional diagnosis on the request can help guide the protocol for imaging investigation. This will help to determine what conditions should be ruled in and out
- relevant history and examination findings: can help indicate the most likely diagnosis as well as the area to focus on
- red flags: make note of any red flags which are indicators for specific clinical suspicion
- availability of previous imaging.
Take a conservative and patient-centred approach to management
A conservative approach to management, which includes a combination of activity modification, physical therapy and symptom-relieving medicines, produces satisfactory results for most patients.29
If analgesia is required, paracetamol should be offered as a first-line option. Non-steroidal anti-inflammatory drugs (NSAIDs) may also be used in combination with or instead of paracetamol if the patient does not find paracetamol alone helpful30 and if there are no contraindications.
Physical therapy can help maintain function of the shoulder joint but should be undertaken with caution,29 so referral to a physiotherapist for specific advice is recommended.30 A supervised exercise regime has demonstrated benefit in both the short and longer term for some patients.31
Establishing a shared understanding with the patient is essential.
Listening to and acknowledging each patient’s concerns and ideas about their shoulder pain can also improve patient satisfaction.32
Choosing Wisely Australia helps healthcare providers and consumers have important conversations about improving the quality of healthcare by reducing unnecessary and sometimes harmful tests, treatments, and procedures.
Led by Australia’s colleges, societies and associations and facilitated by NPS MedicineWise, Choosing Wisely Australia challenges the way we think about healthcare, questioning the notion 'more is always better'.
5 questions to ask your doctor or other healthcare provider is a resource that can help patients ensure they end up with the right amount of care.
See the Choosing Wisely recommendations on shoulder pain
Recommendation from the Australian Rheumatology Association
Expert reviewer
Dr Michael Yelland
General and musculoskeletal medicine practitioner, Arana Hills Medical Centre
Associate Professor, School of Medicine, Griffith University
References
- Brown Z, Shanahan E. Shoulder pain: How to assess, when to refer. Pain Management Today 2018;5:4-11.
- Mitchell C, Adebajo A, Hay E, et al. Shoulder pain: diagnosis and management in primary care. BMJ 2005;331:1124-8.
- Britt H, Miller G, Henderson J, et al. General practice activity in Australia 2015-16. 2016.
- Johal P, Martin D, Broadhurst N. Managing shoulder pain in general practice - assessment, imaging and referral. Aust Fam Physician 2008;37:263-5.
- Artus M, van der Windt DA, Afolabi E, et al. Management of shoulder pain by UK general practitioners (GPs): A national survey. BMJ Open 2017;7:e015711.
- Cleland J, Koppenhaver S, Su J. Netter's orthopaedic clinical examination: An evidence-based approach 2nd ed. Philadelphia, USA: Saunders/Elsevier, 2011.
- Cadogan A, McNair P, Laslett M, et al. Diagnostic accuracy of clinical examination and imaging findings for identifying subacromial pain. PLoS One;11:e0167738.
- Somerville W. Pain in the arm: A symptom of heart disease. Postgrad Med J 1959;35:410-12.
- Neviaser AS, Neviaser RJ. Adhesive capsulitis of the shoulder. J Am Acad Orthop Surg 2011;19:536-42.
- Ngian GS. Rheumatoid arthritis. Aust Fam Physician 2010;39:626-8.
- Kenna C, Murtagh J. Back pain and spinal manipulation: A practical guide. 2nd ed. Sydney: Butterworth-Heinemann, 1997.
- van Hecke O. Polymyalgia rheumatica -- diagnosis and management. Aust Fam Physician 2011;40:303-6.
- Brun S. Initial assessment of the injured shoulder. Aust Fam Physician 2012;41:217-20.
- Buchbinder R, Staples MP, Shanahan EM, et al. General practitioner management of shoulder pain in comparison with rheumatologist expectation of care and best evidence: an Australian national survey. PLoS One 2013;8:e61243.
- Brun S. Shoulder injuries: Management in general practice Aust Fam Physician 2012;14:188-94.
- Girish G, Lobo L, Jacobson J, et al. Ultrasound of the shoulder: Asymptomatic findings in men. AJR Am J Roentgenol 2011;197:W713-9.
- Sher J, Uribe J, Posada A, et al. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 1995;77:10-5.
- Lewis J. Rotator cuff related shoulder pain: Assessment, management and uncertainties. Man Ther 2016;23:57-68.
- Artus M, Holt T, Rees J. The painful shoulder: an update on assessment, treatment and referral. Br J Gen Pract 2014;64:e593–e5.
- Hershkovich O, Shapira S, Sela Y, et al. Role of radiographs in shoulder pathology: a clinical review. Reports in Medical Imaging 2014;7:75-80.
- Ludewig P, Kamonseki D, Staker J, et al. Changing our diagnostic paradigm: movement system diagnostic classification. Int J Sports Phys Therap 2017.
- Ristori D, Miele S, Rossettini G, et al. Towards an integrated clinical framework for patient with shoulder pain. Arch Physiother 2018;8:7.
- Liesdek C, van der Windt DAWM, Koes BW, et al. Soft-tissue disorders of the shoulder: A study of inter-observer agreement between general practitioners and physiotherapists and an overview of physiotherapeutic treatment. Physiotherapy 1997;83:12-7.
- Schellingerhout JM, Verhagen AP, Thomas S, et al. Lack of uniformity in diagnostic labeling of shoulder pain: Time for a different approach. Man Ther 2008;13:478-83.
- Buchbinder R, Goel V, Bombardier C, et al. Classification systems of soft tissue disorders of the neck and upper limb: Do tthey satisfy methodological guidelines? J Clin Epidemiol 1996;49:141-9.
- Broadhurst N, Baghurst T, MacLaren S. Ultrasound imaging for shoulder pain in general practice. Aust Fam Physician 2004;33:668-9.
- NPS Medicinewise. Essentials in an imaging referral. Sydney: NPS MedicineWise, 2015.
- Government of Western Australia. Diagnostic imaging pathways: About imaging: General principles in requesting and providing imaging invstigations. Perth: Government of WA, 2017.
- Burbank K, Stevenson J, Czarnecki G, et al. Chronic shoulder pain: part II. Treatment. Am Fam Physician 2008;77:493-7.
- Rheumatology Expert Group. Therapeutic Guidelines: Limb conditions: Introduction to limb conditions. West Melbourne: Therapeutic Guidelines Ltd, 2017.
- Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev 2003:CD004258.
- Tallman K, Janisse T, Frankel R, et al. Communication practices of physicians with high patient-satisfaction ratings. Perm J 2007;11.
