A balancing act is required when caring for a patient with chronic non-cancer pain.
On one side, you want to optimise the first-line therapies. These include non-pharmacological treatments such as patient education, gradually increasing physical activity and cognitive behavioural therapy (CBT). They may also include non-opioid medicines such as paracetamol and non-steroidal anti-inflammatories (NSAIDs).1,2
On the other side, you want to minimise therapies such as opioids that have a limited role.3,4
Opioids can be an effective component of the management of acute and cancer-related pain. However, evidence shows that for most patients with chronic non-cancer pain, opioids do not provide clinically important improvement in pain or function compared with placebo.3
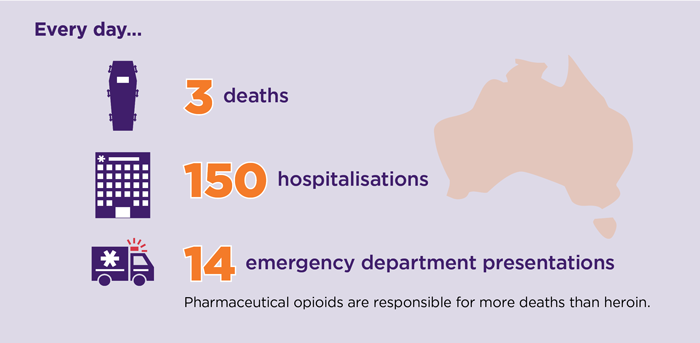
In contrast, they carry significant risk of harm. Around 80% of people taking opioids for 3 months or more experience harms. These range from mild through to severe and fatal.5,6
The bigger picture when treating chronic non-cancer pain
Clinical guidance currently recommends a multidisciplinary approach with an emphasis on non-pharmacological strategies and active self-management as the preferred method to improve function and quality of life.10
This involves using more than one treatment modality from one or more medical disciplines, incorporated into a pain treatment plan. These modalities address the pain condition from a variety of mechanisms, taking a synergistic approach to different aspects of the pain, including improved symptoms and functionality.11 GPs can deliver multimodal care themselves in micro-interventions over multiple consultations.12
The efficacy of a coordinated approach has been recognised to reduce pain severity, improve mood and overall quality of life, and increase function.11 In addition to improving physical function, a biopsychosocial treatment approach to chronic non-cancer pain helps patients understand and overcome secondary effects, including fear of movement, pain catastrophising and anxiety, that contribute to pain and disability.11
Challenges of opioid prescribing
Many factors can influence the decision to prescribe an opioid for chronic non-cancer pain. They may do this either alone or in combination.13
These factors may be grouped into five categories:13,14
- Knowledge about opioids for chronic non-cancer pain
- Experience in the management of chronic non-cancer pain
- Beliefs of the prescriber about opioids and chronic non-cancer pain, such as fear of undertreating pain
- External influences, such as patient pressure to prescribe
- Resources available to healthcare professionals, such as ease of access to physiotherapy or pain specialists
Factors that influence the decision to prescribe may affect health professionals’ perception of the risks associated with their prescribing.13
NPS MedicineWise’s opioids program
It is reasonable to assume that multiple interventions – health professional and consumer education and support, regulatory changes and prescription monitoring – will be needed to get the balance right in the management of chronic non-cancer pain and opioids prescribing in Australia.15
The 2019 NPS MedicineWise program, Opioids, chronic pain and the bigger picture , aims to equip health professionals with tools and resources to reduce the harms of opioids while ensuring adequate pain management and quality of life for patients with chronic non-cancer pain. It also aims to empower consumers to make more informed decisions about opioids.
It aims to make it easier to meet the challenges of opioid prescribing. It will do so through addressing the above factors, enabling health professionals to:
- identify the limited role of opioids and outline the importance of non-pharmacological treatments when managing patients with chronic non-cancer pain
- develop and implement a clear plan with each patient to achieve an improvement in pain and functioning, if an opioid trial is indicated
- review patients who are taking opioids and assess risk of harm and potential benefits to identify patients who would benefit from opioid tapering
- use multidisciplinary services to support patients living with chronic non-cancer pain and identify when to refer patients at high risk of harm from opioids.
References
- Busse JW, Craigie S, Juurlink DN, et al. Guideline for opioid therapy and chronic noncancer pain. CMAJ 2017;189:E659-E66.
- Royal Australian College of General Practitioners. Prescribing drugs of dependence in general practice, Part C2: The role of opioids in pain management. East Melbourne: RACGP, 2017 (accessed 19 March 2019).
- Busse JW, Wang L, Kamaleldin M, et al. Opioids for chronic noncancer pain: A systematic review and meta-analysis. JAMA 2018;320:2448-60.
- Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: The SPACE randomized clinical trial. JAMA 2018;319:872-82.
- Analgesic Expert Group. Therapeutic Guidelines: Analgesic. Version 6. West Melbourne: Therapeutic Guidelines Ltd, 2012 (accessed 10 January 2019).
- Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med 2015;162:276-86.
- Nicholas R. Responding to problems related to pharmaceutical opioids: A resource for prescribers. Adelaide: National Centre for Education and Training on Addiction, 2018 (accessed 21 March 2019).
- Hall T. Opioid analgesic misuse and abuse: an Australian perspective. J Pharm Pract Res 2019;49:3-8.
- Australian Institute of Health and Welfare. Opioid harm in Australia and comparisons between Australia and Canada. Canberra: AIHW, 2018 (accessed 19 April 2019).
- NSW Therapeutic Advisory Group Inc. Preventing and managing problems with opioid prescribing for chronic non-cancer pain. Sydney: NSW TAG, 2015 (accessed 8 January 2019).
- Pain Management Best Practices Inter-Agency Task Force. Draft report on pain management best practices: updates, gaps, inconsistencies and recommendations. Washington DC, USA: US Department of Health and Human Services, 2018 (accessed 18 March 2019).
- Holliday S, Hayes C, Jones L, et al. Prescribing wellness: comprehensive pain management outside specialist services. Aust Prescr 2018;41:86-91.
- Kennedy MC, Pallotti P, Dickinson R, et al. 'If you can't see a dilemma in this situation you should probably regard it as a warning': a metasynthesis and theoretical modelling of general practitioners' opioid prescription experiences in primary care. Br J Pain 2019;13:159-76.
- National Drug and Alcohol Research Centre. A review of opioid prescribing in Tasmania: A blueprint for the future. Sydney: University of New South Wales, 2012 (accessed 21 March 2019).
- Campbell G, Lintzeris N, Gisev N, et al. Regulatory and other responses to the pharmaceutical opioid problem. Med J Aust 2019;210:6-8 e1.