Key points
- General practice has an important role to play in preventing the health burden associated with fractures.
- Many people at high risk of osteoporotic fractures are not identified. Moreover many of these patients remain untreated, even after presenting with a minimal trauma fracture.
- Initiate medicines in patients with a minimal trauma fracture or at higher risk of fracture to prevent future fractures.
- Address issues with adherence to osteoporosis medicines and promote a healthy lifestyle that addresses modifiable risk factors for osteoporosis.
Minimal trauma fracture increases the risk of future fractures
Following an initial minimal trauma fracture, the risk of repeat fractures is doubled.5 This is in addition to the increased risk associated with low bone mineral density (BMD). (Read about all the risk factors for fracture below.)
Higher 5-year mortality rates following repeat fractures
A study found that following an initial minimal trauma fracture, women and men with repeat fractures had higher 5-year mortality rates (39% and 51%, respectively) than people with no repeat fractures (26% and 37%, respectively).6
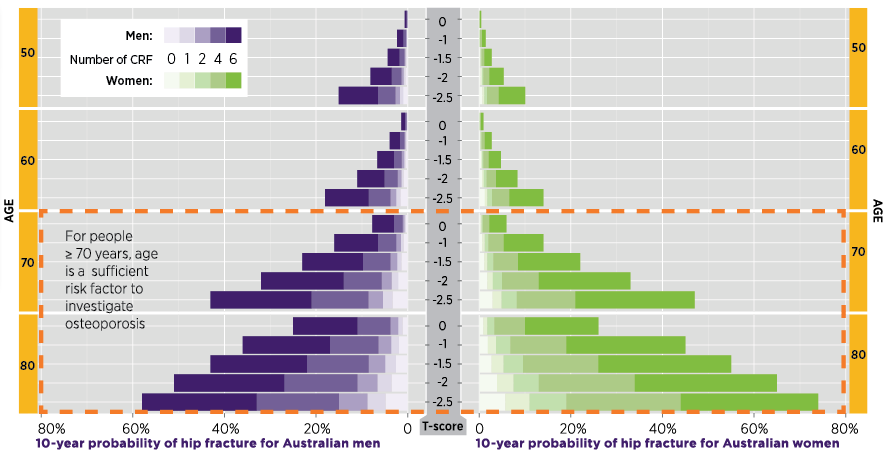
The risk of minimal trauma fracture, particularly hip fracture, increases steeply in older women and men.2,7,9 Highest absolute fracture risk (10% or worse in 3 years) is seen for postmenopausal women and men aged ≥ 70 years with T-scorea < –2.5 (in absence of fracture).2
A minimal trauma fracture is sufficient for a presumptive diagnosis of osteoporosis. Treatment with osteoporosis medicines can start prior to obtaining BMD results with dual energy X-ray absorptiometry (DXA).1,2,9-13
a T-score is the number of standard deviations from a young adult reference mean.
Clinical risk factors and their impact on fracture risk
Risk factors should be assessed14,15 and modifiable risk factors addressed1,2,8,16 in all postmenopausal women aged ≥ 45 years and men aged ≥ 50 years.14,15
A full diagnostic investigation is indicated for:2,15
- women aged > 50 years and men aged > 60 years with multiple clinical risk factors15
- patients aged > 45 years with a minimal trauma fracture or suspected vertebral fractureb,15
- patients who have causes of secondary osteoporosis (medical conditions or medicines such as long-term, high-dose corticosteroidsc)15
- adults aged> 70 years.d,2
Fracture risk increases with decreasing BMD, which is a well-known age-dependent risk factor.14,17 Other clinical risk factors (CRFs) further raise a person's risk of fracture (Figure 1).18-20 This means a 60-year-old man with a T-score of –1.0 and 4–6 risk factors would have a higher 10-year probability of hip fracture than a 70-year-old man with the same T-score and no risk factors other than age (Figure 1).
When assessing an individual’s absolute fracture risk, the relative contribution of these other clinical risk factors needs to be considered.18
Online absolute fracture risk calculators, such as FRAX18,20,21 and Garvan Fracture Risk Calculator,21-23 can assist when discussing fracture risk with patients.
Clinical risk factors in Figure 1 include:
- previous minimal trauma fracture
- oral corticosteroid use
- rheumatoid arthritis
- alcohol intake ≥ 3 units /day
- current smoking
- parental history of hip fracture.
Notes
b PBS defines vertebral fracture as ≥ 20% reduction in the height of the anterior or mid portion of a vertebral body relative to the posterior height of that body or ≥ 20% reduction in any of these heights compared to the vertebral body above or below the affected vertebral body.
c Defined as > 7.5 mg/day of prednisolone or equivalent for > 3 months. MBS subsidy applies only for patients taking this dose for at least 4 months.
d In people aged > 70 years, age is a sufficient risk factor to prompt BMD testing by DXA.
BMD testing by DXA is the gold standard for an osteoporosis diagnosis
DXA scanning is recommended for women aged > 50 years and men aged > 60 years with multiple risk factors for osteoporosis.1,2,24
DXA is the gold standard in Australia for obtaining BMD measures and can assist with diagnosis, monitoring and treatment decisions, and communicating these with patients.25
The WHO criteria utilising T-scores can be used to diagnose osteopenia and osteoporosis (Figure 2).1 Z-scoree is useful for evaluating bone loss in patients aged < 50 years.1,24 Actual BMD (g/cm2) is required for monitoring BMD changes over time.1,26
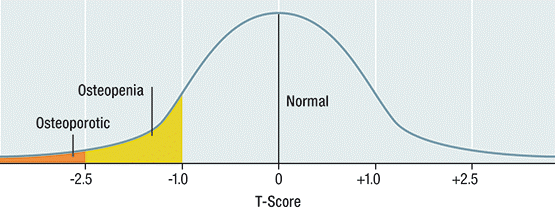
Used with permission from Osteoporosis Australia - Health Professional Guide
Diagnosis should exclude secondary causes
Identify and treat underlying causes for osteoporosis or other medical conditions such as multiple myeloma and metabolic bone disease (eg, osteomalacia, renal bone disease) that may closely simulate osteoporosis.1,2
Laboratory tests are indicated after a minimal trauma fracture, if a patient’s medical history or examination suggests secondary causes, or if a patient's Z-score < –2.0.2
e Z-score is the number of standard deviations from an age- and sex-matched reference mean.
Expert reviewers
- Associate Professor Vasi Naganathan, Centre for Education and Research on Ageing, University of Sydney. Ageing and Alzheimer's Institute, Concord Hospital, Sydney, NSW.
- Dr Simon Vanlint, General Practitioner and Clinical Senior Lecturer, University of Adelaide, Adelaide, SA.
References
- Therapeutic Guidelines. Bone and metabolism. Melbourne: Therapeutic Guidelines Ltd, 2019 (accessed 21 December 2021).
- Royal Australian College of General Practitioners. Clinical guideline for the prevention and treatment of osteoporosis in postmenopausal women and older men. Melbourne: RACGP, 2010 (accessed 30 April 2015).
- Nguyen TV, Center JR, Eisner JA. Osteoporosis: underrated, underdiagnosed and undertreated. Med J Aust 2004;180:S18–22 (accessed 6 March 2017).
- Bleicher K, Naganathan V, Cumming RG, et al. Prevalence and treatment of osteoporosis in older Australian men: findings from the CHAMP study. Med J Aust 2010;193:387-91.
- Kanis JA, Johnell O, De Laet C, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone 2004;35:375-82.
- Bliuc D, Nguyen ND, Nguyen TV, et al. Compound risk of high mortality following osteoporotic fracture and refracture in elderly women and men. J Bone Miner Res 2013;28:2317-24.
- Hippisley-Cox J, Coupland C. Predicting risk of osteoporotic fracture in men and women in England and Wales: prospective derivation and validation of QFractureScores. BMJ 2009;339:b4229 (accessed 6 March 2017).
- Scottish Intercollegiate Guidelines Network. Management of osteoporosis and the prevention of fragility fractures. A national clinical guideline. Edinburgh: SIGN, 2021 (accessed 21 December 2021).
- Pharmaceutical Benefits Scheme. Zoledronic acid. Canberra: PBS (accessed 15 May 2015).
- Pharmaceutical Benefits Scheme. Alendronate. Canberra: PBS (accessed 15 May 2015).
- Pharmaceutical Benefits Scheme. Risedronate. Canberra: PBS (accessed 15 May 2015).
- Pharmaceutical Benefits Scheme. Denosumab. Canberra: PBS (accessed 15 May 2015).
- Pharmaceutical Benefits Scheme. Raloxifene. Canberra: PBS (accessed 15 May 2015).
- National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int 2014; 25:2359–81.
- Royal Australian College of General Practitioners. Guidelines for preventive activities in general practice, 9th edition. Melbourne: RACGP, 2016 (accessed 21 December 2021).
- Australian Medicines Handbook. Drugs affecting bone: osteoporosis. Adelaide: AMH Pty Ltd, 2021 (accessed 21 December 2021).
- Johnell O, Kanis JA, Oden A, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res 2005;20:1185–94.
- Kanis JA, Johnell O, Oden A, et al. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 2008;19:385–97.
- Kanis JA, Oden A, Johnell O, et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 2007;18:1033–46.
- World Health Organization Collaborating Centre for Metabolic Bone Diseases. FRAX WHO Fracture Risk Assessment Tool. United Kingdom: WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield (accessed 30 April 2015).
- Sandhu SK, Nguyen ND, Center JR, et al. Prognosis of fracture: evaluation of predictive accuracy of the FRAX algorithm and Garvan nomogram. Osteoporos Int 2010;21:863–71.
- Garvan Institute of Medical Research. Fracture Risk Calculator. Sydney: Garvan Institute (accessed 30 April 2015).
- Nguyen ND, Frost SA, Center JR, et al. Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int 2008;19:1431–44.
- Healthy Bones Australia. Bone density testing in general practice. Sydney: Osteoporosis Australia, 2015 (accessed 5 January 2022).
- Otmar R, Reventlow SD, Nicholson GC, et al. General medical practitioners' knowledge and beliefs about osteoporosis and its investigation and management. Arch Osteoporos 2012;7:107–14.
- Government of Western Australia. Diagnostic imaging pathways - Osteoporosis (suspected). Western Australia: Government of Western Australia, 2014 (accessed 26 June 2015).

