Focus on anticholinergic burden
Anticholinergic burden is defined as the cumulative effect on a person taking one or more medicines with anticholinergic effects.
Anticholinergic burden is defined as the cumulative effect on a person taking one or more medicines with anticholinergic effects.1
While these medicines are useful to treat many conditions such as depression, dementia with changed behaviour and chronic non-cancer pain,2-4 their broad range of action on the central and peripheral nervous systems can result in unintended adverse effects such as falls, confusion, cognitive decline, dry mouth, constipation and urinary retention.1
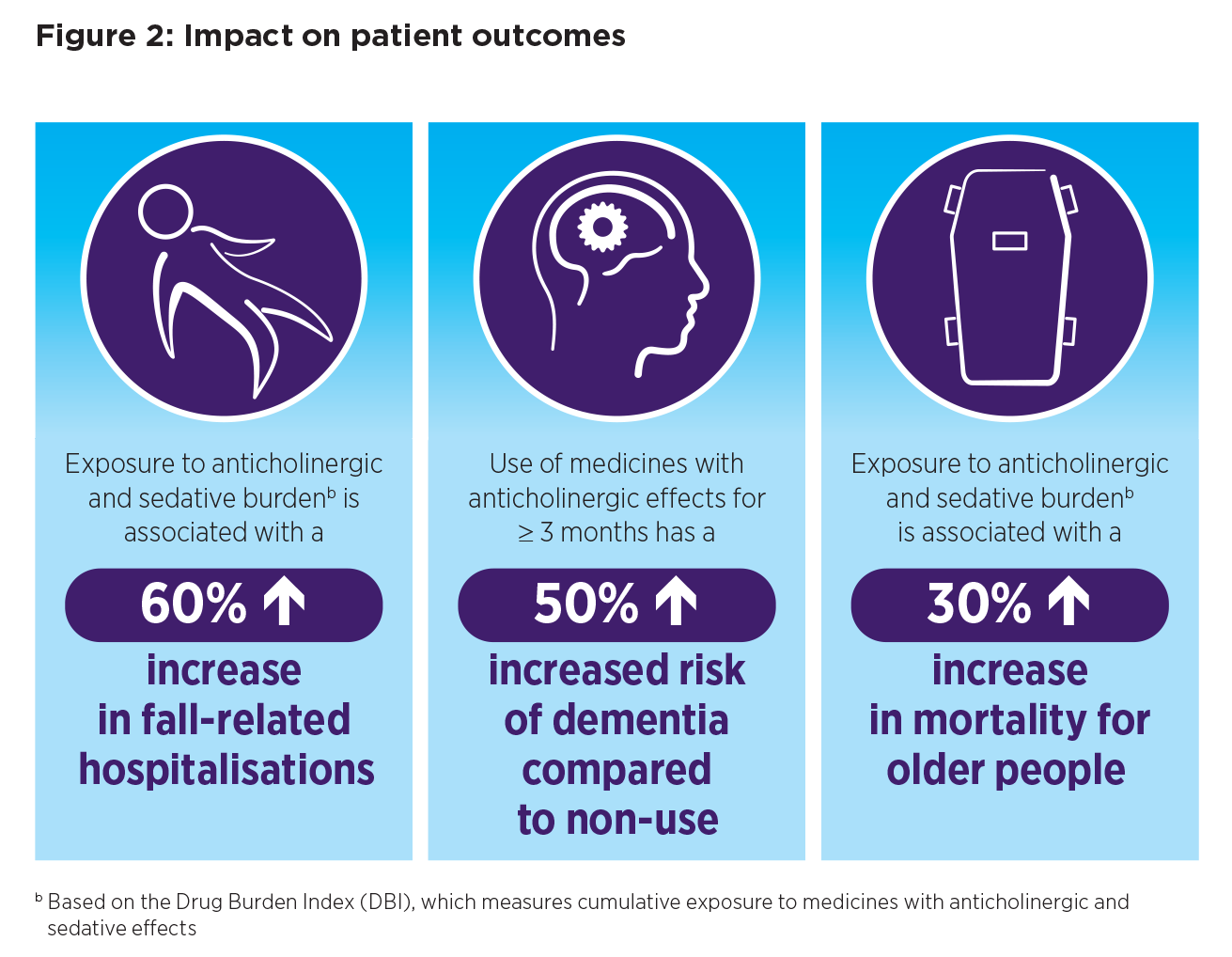
Anticholinergic burden is also associated with poor health outcomes, particularly for older people, including:5,6
- 60% increase in fall-related hospitalisations
- 50% increased risk of dementia
- 30% increase in mortality.
People aged 65 years and older may be more susceptible to anticholinergic burden. Physiological and pathological processes associated with ageing change the size and function of organs that are responsible for the pharmacokinetics and pharmacodynamics of medicines with anticholinergic effects, which may reduce concentrations at which drugs are effective or toxic.1
Compelling reasons to think about anticholinergic burden
The prevalence of polypharmacy among older Australians is relatively high (36%), affecting almost one million older people.7
The NPS MedicineWise Anticholinergic burden: the unintended consequences for older people program aims to improve the health outcomes of older people living in the community and residential aged-care facilities (RACFs) by promoting the safe and effective use of medicines with anticholinergic effects and, as a result, reduce anticholinergic burden.
Key features of the program include educational visits to general practices, and a suite of online resources including online educational activities, clinical resources and tools for health professionals, and factsheets, a decision aid and action plan for patients and their carers.
GPs are ideally placed to identify and manage anticholinergic burden
Identifying and managing medicines with anticholinergic effects can be challenging, as many are not thought of as having anticholinergic effects. Several opportunities that can contribute to improved patient outcomes have been identified, including:
- increasing awareness that certain medicines have anticholinergic effects
- recognising that presenting symptoms such as falls or cognitive decline may be due to anticholinergic burden
- assessing anticholinergic burden
- implementing strategies to reduce anticholinergic burden.
GPs, pharmacists and nurses working across the aged-care sector, in primary care, RACFs and at transitions of care, play a key role in the safe use of medicines with anticholinergic effects.
The NPS MedicineWise Anticholinergic burden: the unintended consequences for older people program aims to strengthen the collaborative effort between health professionals by increasing their knowledge of medicines with anticholinergic effects and how to individualise the approach to reducing anticholinergic burden that is aligned to consumer goals.
References
- Kouladjian O'Donnell L, Gnjidic D, Nahas R, et al. Anticholinergic burden: considerations for older adults. J Pharm Pract Res 2017;47:67-77.
- Australian Medicines Handbook. Adelaide: AMH Pty Ltd, 2021 (accessed 8 July 2021).
- Therapeutic Guidelines. West Melbourne: Therapeutic Guidelines Ltd, 2021 (accessed 23 July 2021).
- The University of Sydney. The goal-directed medication review electronic decision support system G-MEDSS. Sydney: USYD, 2019 (accessed 23 July 2021).
- Nishtala PS, Narayan SW, Wang T, et al. Associations of drug burden index with falls, general practitioner visits, and mortality in older people. Pharmacoepidemiol Drug Saf 2014;23:753-8.
- Dmochowski RR, Thai S, Iglay K, et al. Increased risk of incident dementia following use of anticholinergic agents: a systematic literature review and meta-analysis. Neurourol Urodyn 2021;40:28-37.
- Page AT, Falster MO, Litchfield M, et al. Polypharmacy among older Australians, 2006-2017: a population-based study. Med J Aust 2019;211:71-5.
- Parkinson L, Magin PJ, Thomson A, et al. Anticholinergic burden in older women: not seeing the wood for the trees? Med J Aust 2015;202:91-4.
- Veterans'MATES. Medicines: the hidden contributor to falls and hip fractures. Canberra: Australian Government, 2018 (accessed 6 August 2021).
- Gnjidic D, Cumming RG, Le Couteur DG, et al. Drug Burden Index and physical function in older Australian men. Br J Clin Pharmacol 2009;68:97-105.
- Sittironnarit G, Ames D, Bush AI, et al. Effects of anticholinergic drugs on cognitive function in older Australians: results from the AIBL study. Dement Geriatr Cogn Disord 2011;31:173-8.
