Accessible text and data for Medicines for chronic kidney disease: A practical guide
Accessible data and description of figures relating to the treatment of chronic kidney disease.
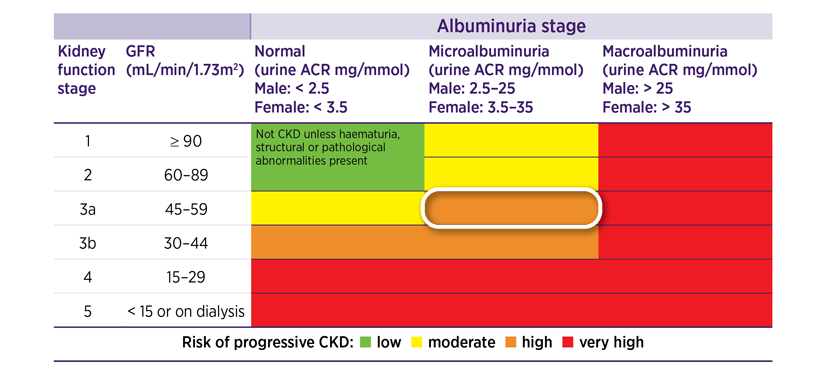
Figure 1 is a colour-coded staging table for kidney function and albuminuria.
Kidney function stage is listed in descending order based on eGFR, down the left side of the table from 1 to 5.
Albuminuria stage based is listed in ascending amount across the top of the table from normo, micro to macro.
The colours are the risk level for CKD progression and cardiovascular events.
Green colour is low risk, yellow is moderate risk, orange is high risk, red is very high risk.
The colour-coded risk levels guide clinical action plans for management.
Back to MedicineWise News
Figure 2: Algorithm for medicines that slow CKD progression and reduce CV risk for people with CKD
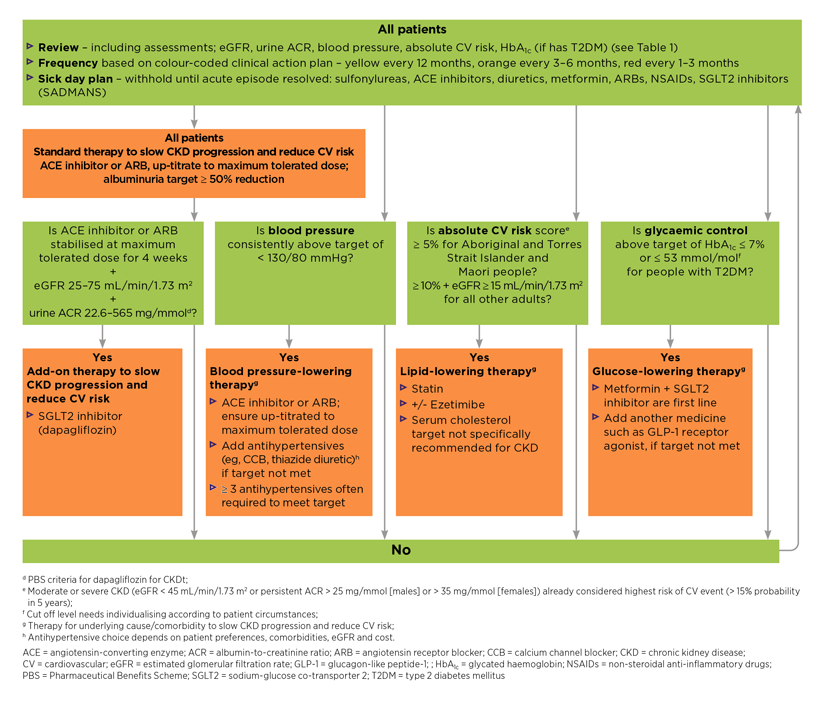
Figure 2 is a flow chart showing the steps for prescribing medicines that slow CKD (chronic kidney disease) progression and reduce CV (cardiovascular) risk for people with CKD, including guideline recommended targets where appropriate.
It starts with explaining that all patients need to have a review that includes clinical and laboratory assessments, with frequency of review based on the colour-coded clinical action plans, and a sick day plan to withhold certain medicines until the acute episode has resolved.
The next step is for all patients to receive standard therapy to slow CKD progression and reduce CV risk, which includes an ACE (angiotensin-converting enzyme) inhibitor or ARB (angiotensin receptor blocker), up-titrated to maximum tolerated dose, with an albuminuria target of 50% or greater reduction.
This is followed by four separate pathways, each pathway conducted for all patients.
The first pathway asks if the ACE inhibitor or ARB has been stabilised at the maximum tolerated dose for 4 weeks, eGFR (estimated glomerular filtration rate) is between 25 and 75 mL/min/1.73 m2 and urine ACR (albumin-to-creatinine ratio) is between 22.6 and 565 mg/mmol.
If the answer is yes, the next step is add-on therapy to slow CKD progression and reduce CV risk with an SGLT2 (sodium-glucose co-transporter 2) inhibitor (dapagliflozin).
The second pathway asks if blood pressure is consistently above the target of less than 130/80 mmHg.
If the answer is yes, the next step is to provide blood pressure-lowering therapy. This includes ensuring an ACE inhibitor or ARB is up-titrated to maximum tolerated dose, adding another antihypertensive medicine such as a CCB (calcium channel blocker) or thiazide diuretic if the target is not met, and that three or more antihypertensives are often required to meet the target.
The third pathway asks if the absolute CV risk score is 5% or more for Aboriginal and Torres Strait Islander and Maori people, or 10% or more as well as if eGFR more than 15 mL/min/1.73 m2 for all other adults.
If the answer is yes, the next step is to provide lipid-lowering therapy with a statin, with or without ezetimibe and that a serum cholesterol target is not specifically recommended for CKD.
The fourth pathway asks if glycaemic control is above the target of HbA1c (glycated haemoglobin) 7% or less, or 53 mmol/mol or less for people with T2DM (type 2 diabetes mellitus).
If the answer is yes, the next step is to provide glucose-lowering therapy, which includes metformin and an SGLT2 inhibitor as first-line treatment and to add another medicine such as a GLP-1 (glucagon-like peptide-1) receptor agonist, if the target is not met.
If the answer is no for any of the four pathways, the next step is to go back to the start of the flow chart.
Table 1: Assessment and management for people with CKD based on colour-coded clinical action plans
| CKD clinical action plansb | eGFR ≥ 60 with microalbuminuria or eGFR 45–59 with normoalbuminuria | eGFR 30–59 with microalbuminuria or eGFR 30–44 with normoalbuminuria | Macroalbuminuria irrespective of eGFR or eGFR < 30 irrespective of albuminuria |
| Frequency of review | Every 12 months | Every 3–6 months | Every 1–3 months |
| Clinical assessments | Oedema | ||
| Laboratory assessmentsb |
| ||
| |||
| Other assessments and measures |
| ||
| |||
| |||
| Non-pharmacological management |
| ||
| Pharmacological management |
| ||
| Reduce doses of medicines that are cleared by the kidneys | |||
b eGFR measures are in mL/min/1.73 m2.
c People with moderate or severe CKD (macroalbuminuria or eGFR < 45) are considered to already be at the highest risk of a CV event, and therefore should not be assessed using the absolute CV tool.
ACR = albumin-to-creatinine ratio; BGL = blood glucose level; BMI = body mass index; CKD = chronic kidney disease; CV = cardiovascular; eGFR = estimated glomerular filtration rate; EUC = electrolytes, urea, creatinine; FBC = full blood count; HbA1c = glycated haemoglobin; NRT = nicotine replacement therapy.