Thiopurines for inflammatory bowel disease
Thiopurines are a type of medicine used to treat Crohn’s disease and ulcerative colitis. They work by reducing the activity of your immune system to help control inflammatory bowel disease (IBD). There are two thiopurines available in Australia. Use this action plan when you are starting thiopurines. It can help you understand the benefits and risks and the need for monitoring and checks.
| Active ingredient | Brand name |
|---|---|
| azathioprine | Azapin, Imazan, Imuran, Thioprine |
| 6-mercaptopurine (6-MP) | Puri-netho |
Taking thiopurines
Benefits
| Fewer flares | Better control of your disease | Reduced need for steroids |
| Better healing of bowel wall | Lower risk of hospitalisation and surgery | Improved quality of life |
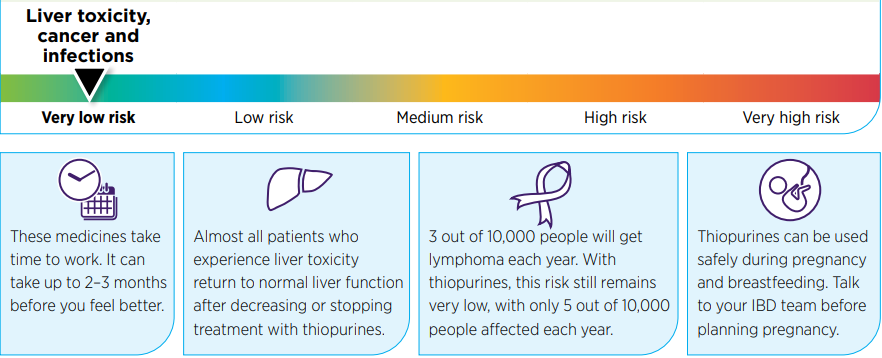
Things to consider
Questions to ask my doctor IBD team
Further information
- Crohn’s & Colitis Australia crohnsandcolitis.com.au
- GESA – Inflammatory bowel disease patient factsheet gesa.org.au
- Download the MedicineWise app to keep track of your medicines and access health information such as blood test results. nps.org.au/medicinewiseapp/
Before starting a thiopurine
| Get blood tests to check your full blood count, liver and kidney function, immunity to certain infections | ||
| Determine your TPMT level (the enzyme activity in your blood that determines how you process, or metabolise, thiopurines). This helps your doctor decide on a suitable dose for you | ||
| Have vaccinations (eg, influenza, pneumococcal, HPV, hepatitis B, varicella-zoster, MMR) | ||
| Get a baseline skin check (adults) |
My thiopurine dosage
| Date started | Medicine name – Active ingredient | Tablet strength (mg) | Number of tablets | How many times per day? |
|---|---|---|---|---|
| azathioprine | ||||
| 6-mercaptopurine (6-MP) |
Regular monitoring and checks
Speak to a doctor about which of these tests and vaccinations you will need once you are taking thiopurines
| Test | How often | Next appointment/notes |
|---|---|---|
| Blood tests, full blood count, electrolytes, liver function tests | At first every 1–2 weeks depending on your result, then every 3 months or as required | |
| Flu | Every year | |
| Pneumonia | Every 5 years | |
| COVID-19 | As directed | |
| Skin check (adults) | Every year |
When to contact my doctor
| Urgently, if I get any of these symptoms | As soon as possible, if I | Regularly, when I |
|---|---|---|
|
|
|
Download the original pdf of this article
Back to Inflammatory bowel disease hub.
