My rheumatoid arthritis is well controlled with a biological or targeted medicine: can I take less medicine?
Your rheumatoid arthritis (RA) is now well controlled with a biological or targeted medicine, so it may be possible to reduce the amount of medicine you take. Find out more about why reducing the amount of medicine you take might be possible, the potential benefits and harms, and things to discuss with your rheumatologist before making your decision.
What are biological and targeted medicines?
These medicines are used to treat RA. Rather than blocking pain, they act on your immune system to reduce inflammation, pain and joint damage.
There are several types of biological and targeted medicines, each targeting or blocking a different part of your immune system.
These medicines are given as an injection under the skin, an infusion (drip into the vein) or a tablet that you swallow.
There are many different biological and targeted medicines, as well as biosimilar medicines, so make sure you know which one you are using:
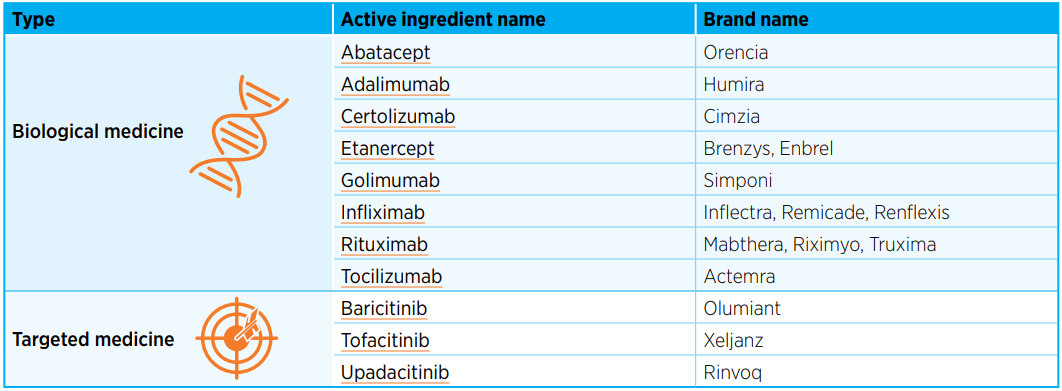
Biological and targeted medicines are not a cure for RA but aim to control the disease.
How do I know if my RA is well controlled?
Well controlled RA means:
- you have no symptoms or only occasional mild symptoms
- your RA doesn’t impact how you feel, move or live your day-to-day life
- your joints are not being damaged by inflammation.
This can also be called ‘being in remission’ or ‘low disease activity’.
Achieving good control of your RA is not a permanent cure and symptoms can reappear throughout your lifetime.
Can I take less biological or targeted medicine when my RA is well controlled?
The goal of treatment is to keep your arthritis well controlled.
Most people will need to continue taking biological or targeted medicines to control their RA.
If your RA is under control for at least 6 months with these medicines, you and your rheumatologist can decide together whether you can:
- continue taking the same amount of biological or targeted medicine, or
- carefully reduce the amount of these medicines you take.
This is a decision for you and your rheumatologist to make together and will depend on how you feel about what’s involved.
What are the potential benefits of taking less biological or targeted medicine?
Potential benefits include:
- fewer injections or infusions
- convenience of taking less medicine
- reduced cost.
What are the potential problems if I take less medicine?
Potential problems include:
- going back to less well controlled RA
- experiencing more pain, inflammation and damage
- experiencing a flare
- being unable to do your usual daily activities.
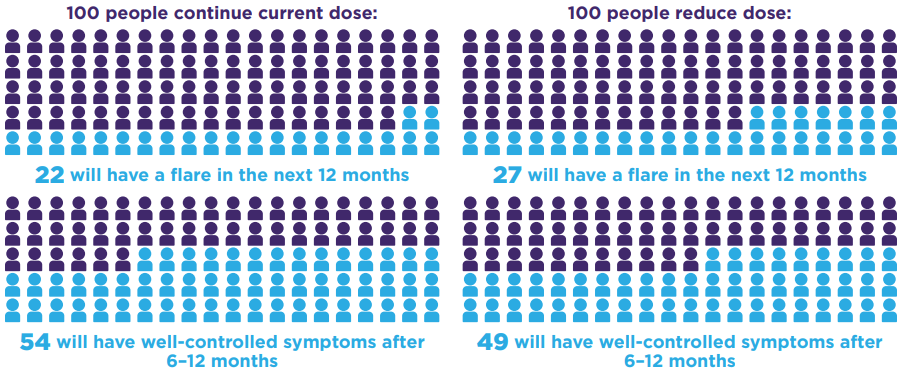
How likely is it that my RA will worsen or flare up if I take less medicine?
Clinical studies have shown there is little or no difference in how well symptoms are controlled or the chance of the disease flaring up when people with well-controlled RA continue using the same dose or reduce the amount of biological or targeted medicine they use.
What happens if my symptoms are still well controlled after reducing my dose?
Your rheumatologist may reduce the dose of these medicines further. Stopping these medicines completely is uncommon and most people with RA will continue taking a biological or targeted medicine throughout their life.
- Your rheumatologist may reduce the amount of other medicines you take for your RA.
- You will need regular, ongoing monitoring for signs of disease activity, such as blood tests and scans, as joint damage can occur without symptoms.
- It can be useful to keep a health diary to track your symptoms.
What happens if my symptoms worsen after reducing my dose?
Your rheumatologist will increase your biological or targeted medicine to the amount you were previously using.
You may also restart or begin other RA medicines to regain control of your symptoms.
Most people (more than 8 in 10) are able to regain good control of their RA after going back to their previous dose or restarting treatment.
This may take some time and it can be useful to keep a health diary to track your symptoms and follow your Flares action plan.
www.nps.org.au/bdmards/rheumatological-conditions.
Keep using your usual pain management techniques, exercising regularly and looking after your mental health.
Where can I get more information?
- Talk to your rheumatologist or rheumatology nurse
- Contact Arthritis Australia at arthritisaustralia.com.au
- Work through the My rheumatoid arthritis is under control: What should I do about my medicine decision aid with your rheumatologist. This tool can help you feel better informed about your options and clearer about what matters most to you when making your decision about your treatment. www.nps.org.au/bdmards/rheumatological-conditions
Download the original pdf of this article
Back to Inflammatory arthritis hub
