Supporting patients with codeine dependence
Clinical advice for clinicians dealing with patients who request codeine and may be codeine-dependent.
Summary
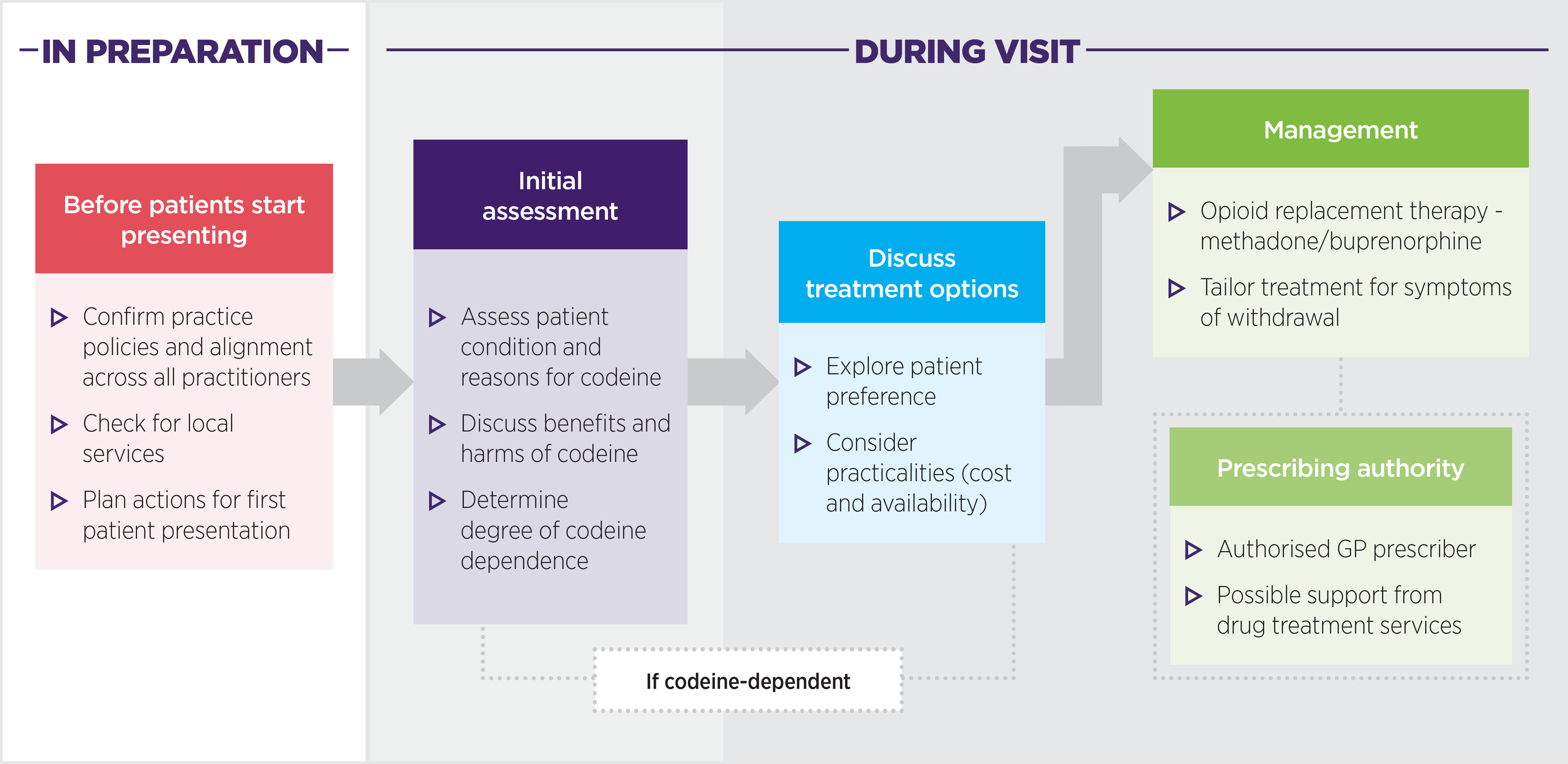
In preparation
Before patients start presenting:
- Confirm practice policies and alignment across all practitioners
- Check for local services
- Plan actions for first patient presentation
During visit
Initial assessment:
- Assess patient condition and reasons for codeine
- Discuss benefits and harms of codeine
- Determine degree of codeine dependence
If the patient is codeine-dependent, take the following steps.
Discuss treatment options:
- Explore patient preference
- Consider practicalities (cost and availability)
Management:
- Opioid replacement therapy - methadone/buprenorphine
- Tailor treatment for symptoms of withdrawal
Prescribing authority:
- Authorised GP prescriber
- Possible support from drug treatment services
Download and print this information
Before patients start presenting
Prepare before a patient presents. Know what you will do and who can support you.
See RACGP Prescribing drugs of dependence in general practice, Part A (section 3.7).
Check your practice policies on drugs of dependence (including codeine). Take positive and definitive action to ensure whole of practice agreement and alignment. RACGP provides guidelines and example policies.
Check your local PHN healthcare pathways for local services.
Check with your state/territory clinical advisory service (see over) to answer any questions you may have before a patient with codeine dependence presents, such as:
- How do I make a referral to a drug treatment service?
- What does the patient need to do after GP referral?
- What is the general waiting time to be seen?
- What are the recommendations to help the patient until they are seen by the drug treatment service?
Initial assessment
Take a non-judgmental stance when assessing the patient’s condition and reasons for taking codeine – the patient’s behaviour is neither good nor bad.
Information that can support next steps may include:
- How has codeine been used, at what dose or frequency and over what period of time?
- Has the dose increased over time?
- Has codeine been used for conditions for which there is no indication?
- Are there symptoms if a dose is missed?
Dependency is a possible adverse effect of opioids (including codeine). Other possible adverse effects include sedation and constipation. Frame the conversation around balancing the potential benefits of codeine therapy (pain relief) with the harms (dependency, sedation, constipation, etc).1
Start with a broad scope and let the patient speak. Use open questions to find out attitudes toward medicines in general and codeine more specifically. Avoid “yes/no” style questions and give them the chance to explain their perception of their medicine use. Some examples are:
- What do your medicines mean to you?
- How do you feel these medicines help you?
- Are you worried about your codeine use?
- When you made the appointment, what were you hoping for?
Explore warning signs of codeine dependence – listen for conversation cues suggestive of dependence and expand on these further. Some examples are:
- Have you ever taken your pain medicines for other reasons?
- Have you ever taken them to help you sleep? When under stress? After a fight with a partner or loved one?
Drug misuse behaviours can include persistently complaining about the need for a drug, asking for specific drugs by name, requesting to have the dose increased, hoarding drugs, pharmacy shopping, unwillingness to consider other drugs and treatments.2,3
Read more: Dealing with drug-seeking behaviour, Australian Prescriber 2016;39:96-100.
Patients with codeine dependence may not self-identify as ‘people who use drugs’. They may be socially advantaged with high achievements in education, adequate social supports and good incomes.3
Discuss treatment options
Explore the patient’s treatment preferences and willingness to change, explaining the expected outcomes of the different options. Patients may be reluctant to commence opioid replacement therapy due to the stigma and negative perception of these treatments4 and may want to withdraw from opioid use without understanding the likelihood of success.
Ensure the practicalities of treatment (including cost and access to treatment) are considered.5
Management
Pharmacotherapy or opioid replacement therapy (ORT) is an effective treatment for opioid dependence.6 Methadone and buprenorphine have been used to treat opioid dependence, both in detoxification from opioids and as maintenance treatment.6 ORT is not suitable for every patient.7
Prescribers must have relevant state or territory authority (see below).2
Consider medicines that can help to alleviate unpleasant symptoms of withdrawal such as anti-emetics for nausea or loperamide for diarrhoea. Coping strategies may also be beneficial to support withdrawal.
Tapering is not recommended as a standalone treatment for codeine dependence. Compared to ORT, tapering appears to be associated with poorer outcomes, including risk of overdose.4,8,9
Clinical advisory services (see below) can be consulted for referral to a drug treatment service and for advice on interim treatment before referral.
The cost of ORT is fully funded under the PBS, although there may be a pharmacist-supervised dispensing fee.7
Prescribing authority
Drugs of dependence cannot be prescribed for patients with known or suspected dependence without a permit or an appropriate approval from the relevant State or Territory health department pharmaceutical services unit (PSU).
Read more, including links to State/Territory relevant fact sheets: RACGP Prescribing drugs of dependence in general practice, Part A (section 2.1)
State and Territory clinical advisory services
- ACT: DACAS – 03 9418 1082
- New South Wales: DASAS – 02 9361 8006 (Sydney Metropolitan), 1800 023 687 (regional and rural NSW)
- Northern Territory: DACAS – 1800 111 092
- Queensland: MRQ (8am –8pm 7 days) 137 846
- South Australia: DACAS – 08 7087 1742
- Tasmania: DACAS – 1800 630 093
- Victoria: DACAS – 1800 812 804
- Western Australia: CAS – 08 9442 5042
Drug and Alcohol Clinical Advisory Service (DACAS), Clinical Advisory Service (CAS), Medicines Regulation and Quality (MRQ), Drug and Alcohol Specialist Advisory Service (DASAS)
Expert reviewers
Dr Penny Abbott
Senior Lecturer, General Practice
School of Medicine, Western Sydney University
Dr Adrian Reynolds
Clinical Associate Professor
President of the Chapter of Addiction Medicine, RACP
References
- Nicolaidis C. Police officer, deal-maker, or health care provider? Moving to a patient-centered framework for chronic opioid management. Pain Med 2011; 12: 890-7.
- Royal Australian College of General Practitioners, Prescribing drugs of dependence in general practice, Part A. East Melbourne.: RACGP 2015.
- James J. Dealing with drug-seeking behaviour. Aust Prescr 2016; 39: 96-100.
- Frei M. Opioid dependence - management in general practice. Aust Fam Physician 2010; 39: 548-52.
- Nielson S, Cameron J, Pahoki S. Over the counter codeine dependence: final report. Melbourne: Turning Point, 2010.
- Department of Health and Human Services (Vic). Maintenance pharmacotherapy. Melbourne: DHHS, (accessed 24 November 2017).
- McDonough M. Opioid treatment of opioid addiction. Aust Prescr 2013; 36: 83-7.
- Wines JD Jr, Saitz R, Horton NJ et al. Overdose after detoxification: a prospective study. Drug Alcohol Depend 2007; 89: 161-9.
- Digiusto E, Shakeshaft A, Ritter A et al. Serious adverse events in the Australian National Evaluation of Pharmacotherapies for Opioid Dependence (NEPOD). Addiction 2004; 99: 450-60.
