Practice Review – Abdominal imaging
Optimising imaging referrals for chronic abdominal pain
Australian GPs recently received a Practice Review on abdominal imaging. This Practice Review is intended to help GPs reflect on referrals for selected MBS imaging services of the abdomen and pelvis. It was developed in collaboration with GPs and has been sent to approximately 30,000 medical practitioners nationally, including all GPs.
The information on this page may help GPs interpret their individual Practice Review data. National and aggregate data for different remoteness area (RA) classifications are included below.
Download and print a sample report
Frequently asked questions
Data from across Australia
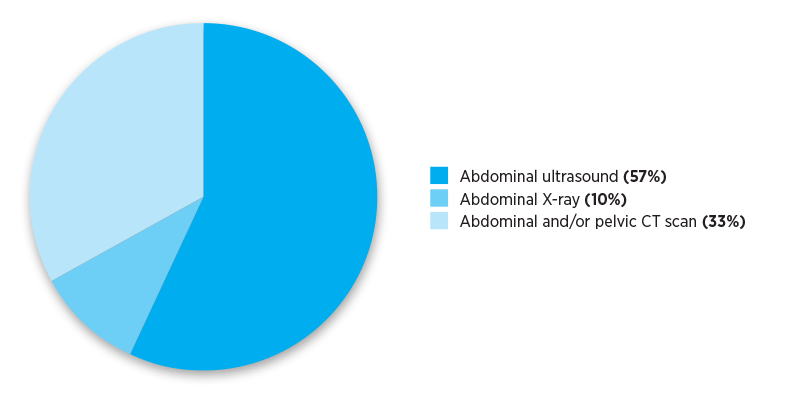
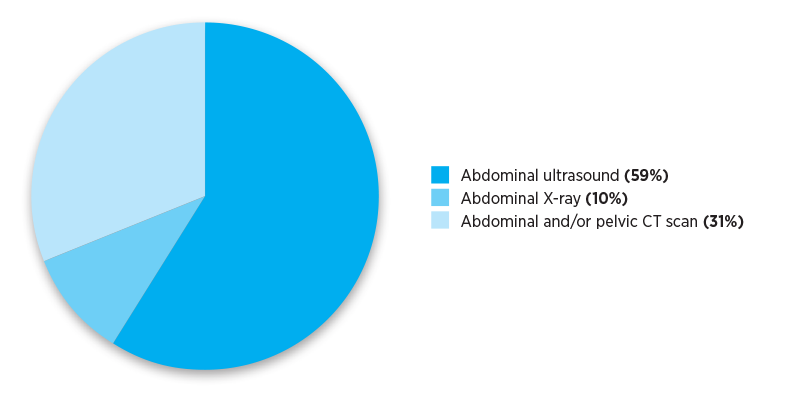
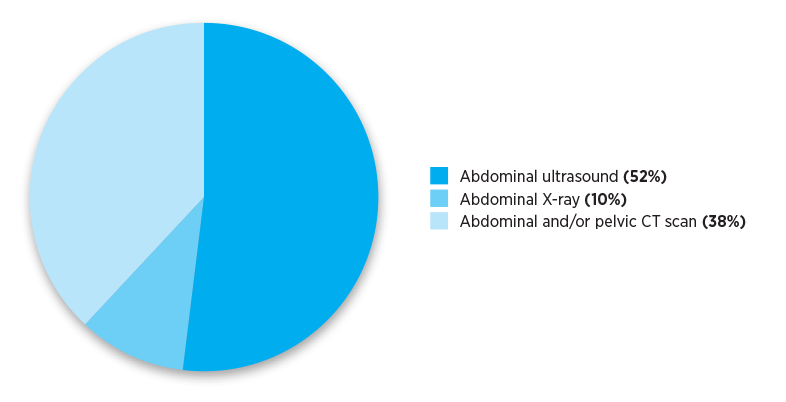
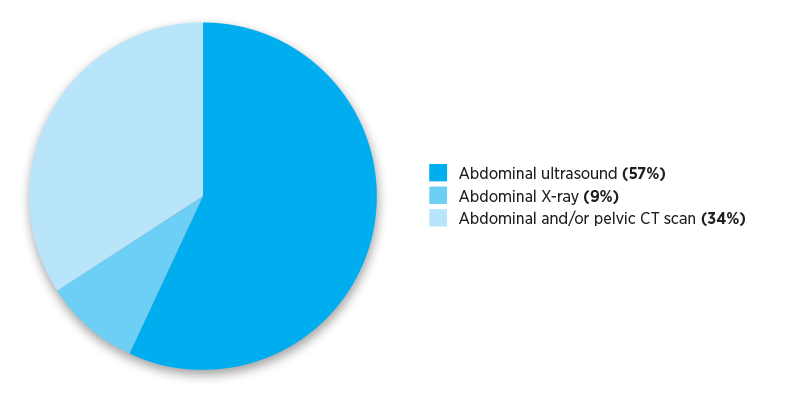
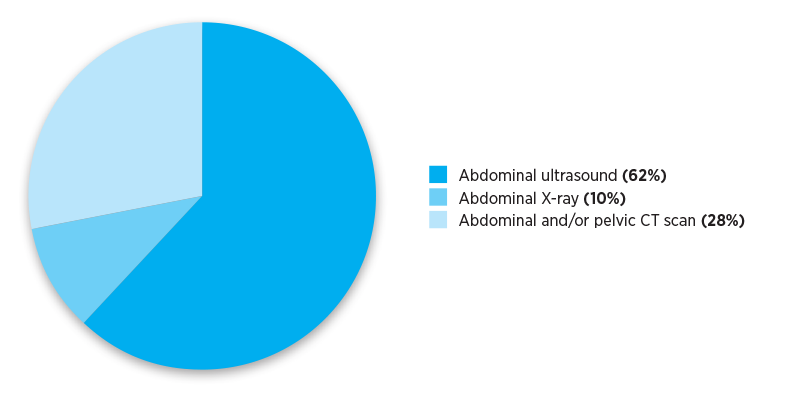
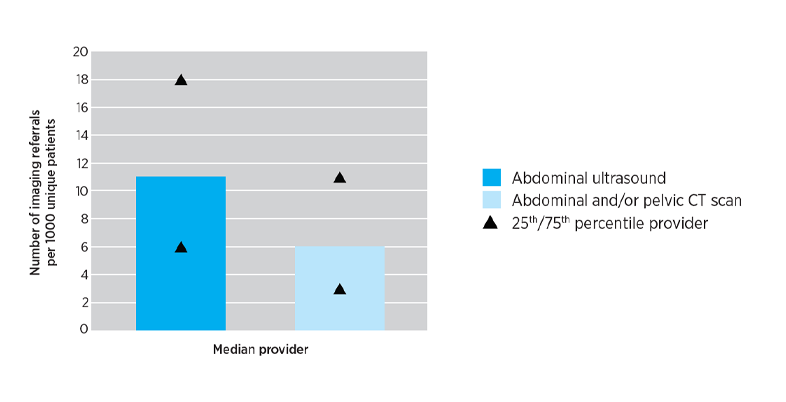
The Practice Review that GPs received reported their individualised imaging referral data. The pie charts below show national and aggregate data for different RA classifications. The data show numbers of referrals for selected abdominal and pelvis MBS imaging services written by Australian medical practitioners in the calendar year 2019.
Points for reflection
- Taking a clinical history and performing a physical examination is the first step when a patient presents with chronic abdominal pain.1
- Diagnostic imaging pathways such as WA Diagnostic Imaging Pathways are available and may be helpful to determine whether imaging is indicated and if so, the most appropriate imaging type.
- Balance the benefits and harms of imaging when indicated. (See below for information about benefits and harms).
- When imaging is required, ensure that referrals include information on specific location to image and suspected condition, to focus the investigation and assist in interpreting results.2
- Read more about quality referrals
Balance the benefits and harms of imaging
When referring a patient for imaging, consider the benefits and harms of each type of imaging to determine which is the most appropriate. These include:
- the specific needs of the investigation
- the patient’s ionising radiation dose
- management of any incidental finding
- the consequences of overdiagnosis.
Consider which imaging modality is best for answering the specific clinical question and minimising the risk of harms.
For example, if a CT scan of an organ is being considered, balance the benefits of enhanced image quality of a CT scan against the risk of harms associated with the ionising radiation, compared to an ultrasound, which does not contain any ionising radiation.3
Although X-rays are rarely indicated for investigating chronic abdominal pain,4 they are associated with much lower doses of ionising radiation than CT scans and so should be considered where appropriate.5
For example, the ionising radiation dose from an abdominal X-ray of the stomach is at least 50 times smaller than the dose from an abdominal CT scan.5
Find out more about managing the risk of exposing patients to ionising radiation
Increased use of modalities associated with high imaging quality such as CT scans increases the risk of incidental findings.6
The American College of Radiography provides information about incidental findings
This information is available to help radiologists make informed decisions when reporting on imaging tests and also to help medical practitioners manage incidental findings.
Overdiagnosis is a harmful and costly problem with two major causes: overdetection and overdefinition of disease. While the forms of overdiagnosis differ, the consequences are the same: diagnoses that ultimately cause more harm than benefit.6
Useful resources
- Pichetshote N, Pimentel M. An approach to the patient with chronic undiagnosed abdominal pain. Am J Gastroenterol 2019;2019:726-32.
- Mendelson R. Imaging for chronic abdominal pain in adults. Austr Prescr 2015;38:49-54.
- Berland LL, Silverman SG, Gore RM, et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol 2010;7:754-73.
References
- Pichetshote N, Pimentel M. An approach to the patient with chronic undiagnosed abdominal pain. Am J Gastroenterol 2019;2019:726-32.
- Mendelson R. Imaging for chronic abdominal pain in adults. Aust Prescr 2015;38.
- Radiological Society of North America. Computed Tomography (CT) - Abdomen and Pelvis. Oak Brook, Illinois, USA: RSNA, 2018 (accessed 28 February 2020).
- Diagnostic Imaging Pathways. Perth: Government of Western Australia Department of Health, 2014 (accessed 4 February 2020).
- Brenner DJ, Hall EJ. Computed tomography - An increased source of radiation exposure. N Engl J Med 2007; 357:2277-2284.
- Brodersen J, Schwartz LM et al. Overdiagnosis: what it is and what it isn’t. BMJ Evid Based Med 2018; 23:1-3.