Key points
- Targeted screening of people at risk of developing CKD is critical for early detection and timely management of this silent disease.
- Screening includes a blood test for serum creatinine to calculate estimated glomerular filtration rate (eGFR), a urine albumin- creatinine ratio (ACR) test and blood pressure check. These 3 components complete a Kidney Health Check.
- A diagnosis of CKD is confirmed if there is a reduction in eGFR (< 60 mL/min/1.73 m2) for ≥ 3 months and/or elevated ACR (males ≥ 2.5 mg/mmol, females ≥ 3.5 mg/mmol) for ≥ 3 months.
- After confirming a diagnosis of CKD, further investigations may help determine the underlying pathology.
- Complete documentation of a CKD diagnosis requires recording the stage (based on eGFR result), level of albuminuria (based on ACR) and underlying cause.
- Timely management reduces both the burden of kidney failure and the associated cardiovascular morbidity and mortality.
One in 10 Australian adults have signs of probable chronic kidney disease (CKD).1,2 For Aboriginal and Torres Strait Islander peoples, the prevalence is even higher, affecting nearly one in five adults.3 CKD contributes to 11% of all deaths and is associated with 33% of all cardiovascular deaths in Australia.4
However, the asymptomatic nature of CKD means it can be difficult to diagnose unless there is targeted screening for it. Timely management can slow or even prevent the deterioration in kidney function, and improve cardiovascular outcomes.1,5,6
GPs are in a prime position to detect and diagnose CKD early. This involves targeted screening and performing investigations that are mostly already part of regular clinical practice.1
Download and print
What is CKD?
The Kidney Health Australia CKD Management in Primary Care handbook defines CKD as:1,5
- reduced kidney function for ≥ 3 months as demonstrated by:
- estimated or measured glomerular filtration rate (GFR) < 60 mL/min/1.73 m2,
and/or
- kidney damage for ≥ 3 months as demonstrated by:
- albuminuria (elevated urine albumin/creatinine ratio [ACR]), or
- haematuria after the exclusion of urological causes, or
- structural abnormalities, such as those found on kidney imaging tests, or
- pathological abnormalities, such as those found on kidney biopsy.
What are the causes?
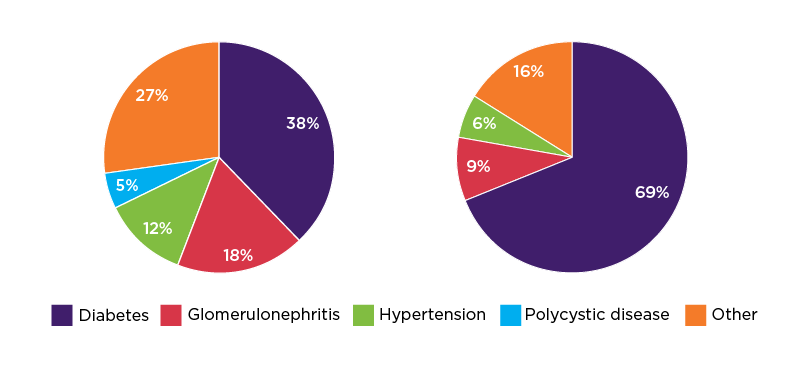
The most common causes of CKD among Australian adults with kidney failure (end-stage kidney disease) are diabetes (38%), glomerulonephritis (18%) and hypertension (12%).7 See Figure 1a.
For Aboriginal and Torres Strait Islander adults with kidney failure, the most common causes are diabetes (69%), glomerulonephritis (9%) and hypertension (6%).7 See Figure 1b.
Why is CKD an important clinical issue?
The morbidity and mortality data on CKD are concerning. CKD is twice as common as diabetes among Australian adults (see Figure 2).8
People with CKD (stage 3 and 4) face the same risk of myocardial infarction as people with diabetes.9 More than one in four (29%) Australian adults have CKD, diabetes or cardiovascular disease (CVD).8
More Australians die every day due to CKD compared with breast cancer and prostate cancer.1,10
The risk of dying from CVD is 50% greater for a 70 year old and 240% greater for a 50 year old with CKD, compared with people of the same age without CKD.11
People with CKD living in remote and very remote areas are three times more likely to go to hospital (excluding for regular dialysis) and almost twice as likely to die compared with those living in major cities.4
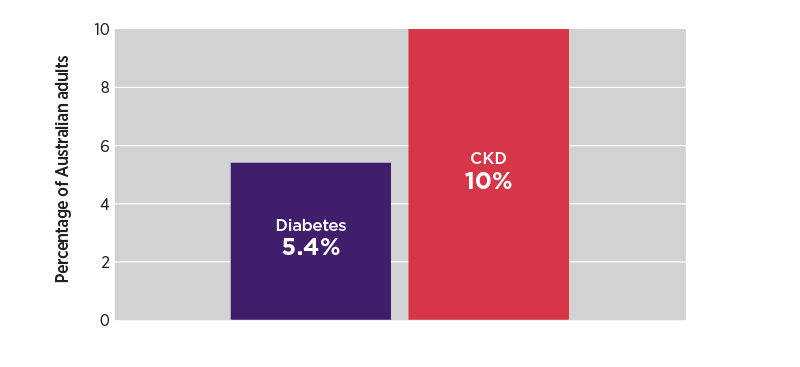
Figure 2: CKD and diabetes prevalence rates among Australian adults (> 18 years)8
Data based on Australian Institute of Health and Welfare material
A silent disease
Due to the asymptomatic nature of CKD,1,6 less than 10% of people affected are aware they have the condition. By the time they become aware, 65.3% of people with CKD have already progressed to stages 3–5.2 For more information about kidney function stages see ‘Colour-coded CKD staging table guides management’ section below.
Moreover, Aboriginal and Torres Strait Islander peoples are four times more likely to have stages 4–5 CKD than other Australians.3
There is evidence of low awareness of CKD among the general public12 and deficiency of knowledge about CKD, including risk factors and guidelines for screening, among health professionals.13
Other challenges in clinical practice include the perception that the multiple comorbidities associated with CKD are too complex to manage within time constraints, and other comorbidities often take priority in consultations.14
Communication barriers can also contribute to the lack of awareness of a CKD diagnosis among patients, due to the perception by some health professionals that providing a diagnosis is an unnecessary mental burden for sufferers.14
Initial detection of probable CKD is achieved through targeted screening of individuals with specific risks via a Kidney Health Check.1 The components of a Kidney Health Check are discussed below.
The CKD risk factors that should prompt screening via a Kidney Health Check are often identifiable in the primary care setting (see Table 1). For example, 22% of Australian adults have CVD (including hypertension, heart disease, stroke or heart failure) and 5.4% have diabetes.8
For Aboriginal and Torres Strait Islander peoples there are specific recommendations for screening based on age groups and CKD risk factors (see Table 2). Updated Caring for Australian and New Zealanders with Kidney Impairment (CARI) Guidelines are expected to be released later in 2022.
It is recommended by the RACGP to use the standard question: 'Are you of Aboriginal or Torres Strait Islander origin?' to identify, record and report the Aboriginal and Torres Strait Islander status of patients in general practice.
For non-Indigenous Australians, being aged ≥ 60 years places an individual at increased risk of developing CKD, but in the absence of other risk factors it is not a prompt to routinely do a Kidney Health Check.1
As part of routine care for non-Indigenous Australians aged 45–74 years, an assessment of absolute CVD risk, and for those aged ≥ 40 years, an assessment for type 2 diabetes, are also recommended.16
Table 1: Risk factors that should prompt a Kidney Health Check and recommended screening frequency1
| Risk factorsa | Kidney Health Check frequency |
| Diabetes | Once a year |
| Hypertension | |
| Established cardiovascular diseaseb
| Every 1–2 years |
| Family history of kidney failure | |
| Obesity (BMI ≥ 30 kg/m2) | |
| Smoker | |
| History of acute kidney injury |
a Non-Indigenous Australians aged ≥ 60 years have an increased risk of developing CKD, but in the absence of other risk factors, they do not need to routinely do a Kidney Health Check.
b Established cardiovascular disease is defined as a previous diagnosis of coronary heart disease, cerebrovascular disease or peripheral vascular disease.
Source: Chronic Kidney Disease (CKD) Management in Primary Care (4th edition). Kidney Health Australia, Melbourne, 2020.
Table 2: CKD screening recommendations for Aboriginal and Torres Strait Islander peoples1
| Age/CKD risk factors | Actions required | Frequency |
| 18–29 years (no CKD risk factors) | Screen for CKD risk factors; see Table 1 | Once a year, for example, as part of an annual health assessment |
| 18–29 years (≥ 1 CKD risk factors) | Kidney Health Check | Every 2 years or more frequently if CVD risk is elevated |
| ≥ 30 years regardless of CKD risk factors |
Source: Chronic Kidney Disease (CKD) Management in Primary Care (4th edition). Kidney Health Australia, Melbourne, 2020.
What does a Kidney Health Check involve?
The initial detection of probable CKD is made with a Kidney Health Check.1 See Figure 3.
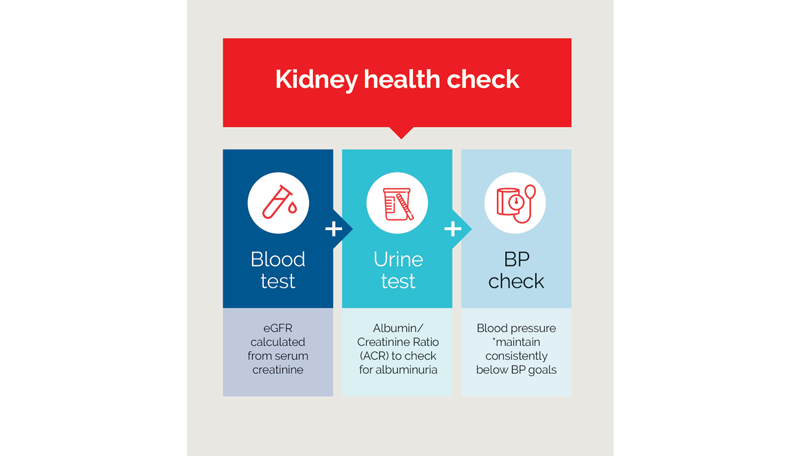
Figure 3: Kidney Health Check1
BP = blood pressure; eGFR = estimated glomerular filtration rate
Source: Chronic Kidney Disease (CKD) Management in Primary Care (4th edition). Kidney Health Australia, Melbourne, 2020.
Read an accessible version of the data in this figure
The GFR provides the best overall measure of kidney function. Estimated (eGFR) is determined from serum creatinine using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) prediction equation.1 The CKD-EPI has been validated for Aboriginal and Torres Strait Islander peoples17 and people of South-East Asian, African, Indian and Chinese descent living in Western countries.18 eGFR is automatically reported with requests for serum creatinine in individuals aged ≥ 18 years.1
The urine ACR test provides the best measure of kidney damage. It detects excessive amounts of albumin in the urine (albuminuria). An elevated ACR is associated with important clinical outcomes independent of eGFR and traditional CVD risk factors such as smoking and cholesterol. Elevated ACR is a strong predictor for risk of cardiovascular disease and progression of CKD in population studies.1,19
Hypertension is a strong risk factor for CKD. Conversely, CKD may also be a cause of hypertension.20 Only one blood pressure (BP) measurement is required for the Kidney Health Check, but regular BP monitoring of individuals at risk of hypertension and/or CKD is encouraged.1,5
What does confirming a diagnosis involve?
It’s recommended to perform the eGFR and ACR tests according to a diagnostic algorithm to confirm a diagnosis of CKD. See Figure 4.
eGFR testing1,21
If 1st test finds reduced eGFR (< 60 mL/min/1.73 m2)
- perform 2nd test within 7 days to exclude acute kidney injury (AKI) as the cause of rapid eGFR decline.
If eGFR is still < 60 mL/min/1.73 m2
but stable (less than 20% change)
- perform a 3rd test at least 3 months later.
If 3rd test finds < 60 mL/min/1.73.m2
(ie, stable reduction)
- CKD is confirmed.
ACR testingc 1,21
If 1st test result shows elevated ACR (males ≥ 2.5 mg/mmol, females ≥ 3.5 mg/mmol)
- perform 2nd test at least 3 months later.
If ACR is still elevated
- CKD is confirmed.
If ACR is not elevated after 2nd test
- perform 3rd test as soon as clinically appropriate.
If at least two out of the three ACR tests over at least 3 months show elevated ACR
- CKD is confirmed.
c first morning void and mid-stream specimen preferable
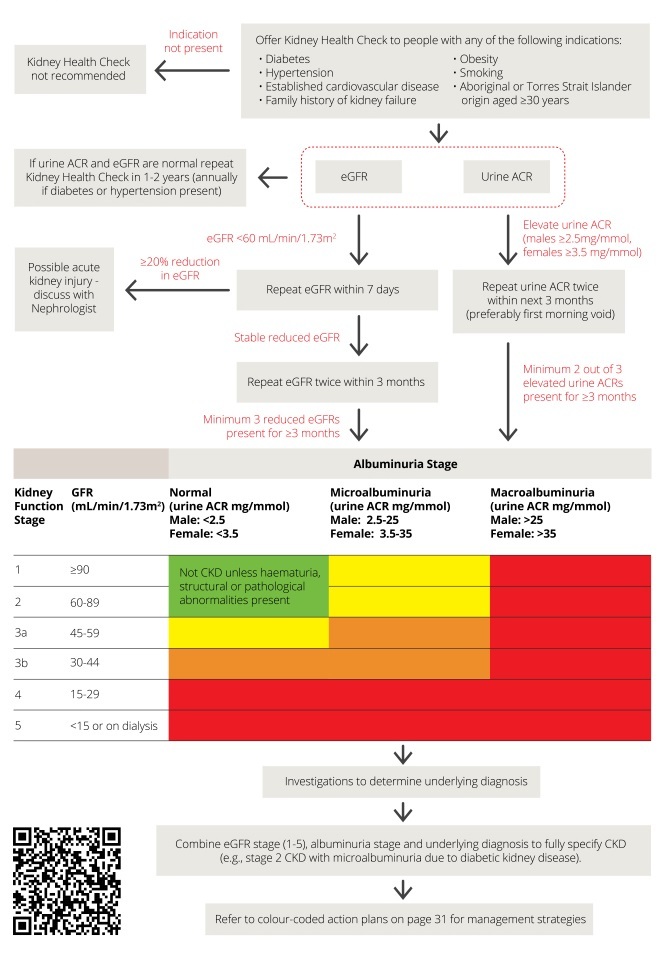
Figure 4: Diagnostic algorithm for CKD1
Source: Chronic Kidney Disease (CKD) Management in Primary Care (4th edition). Kidney Health Australia, Melbourne, 2020.
Read an accessible version of the data in this figure
Practical guidance
Available evidence and clinical practice data suggest that the eGFR and BP check are done well in primary care for people with CKD. However the ACR test is often missed.22
To help bridge practice gaps and overcome time constraints, GPs can consider using existing tools and services such as the Medicare Benefit Schedule’s (MBS) Health Assessments where appropriate.5,23
Further investigations for new diagnosis of CKD
After confirming a diagnosis of CKD there are further investigations that are recommended to help determine the underlying pathology and other comorbidities. These investigations include:1
- blood tests:
- full blood count (FBC)
- electrolytes, urea and creatinine (EUC)
- fasting lipids
- fasting glucose or HbA1c
- erythrocyte sedimentation rate, C-reactive protein
- urine microscopy for dysmorphic red cells, red cell casts or crystals
- renal ultrasound.
Other investigations for the underlying pathology may be indicated depending on the patient’s clinical features.1
Appropriate recording of CKD in the patient record should include the eGFR stage, albuminuria level and underlying cause. See Figure 5.
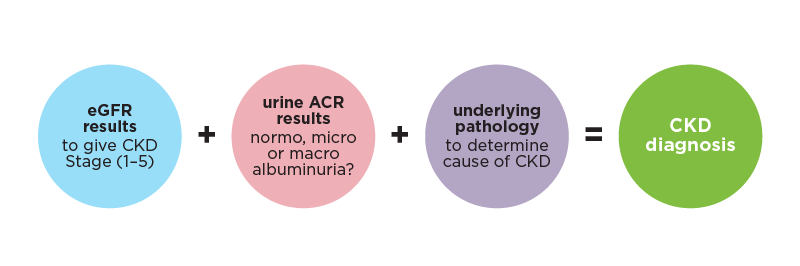
Figure 5: Three components for recording a diagnosis of CKD1
ACR = albumin/creatinine ratio; CKD = chronic kidney disease; eGFR = estimated glomerular filtration rate
An example of how to describe and record a confirmed CKD diagnosis is ‘stage 3 chronic kidney disease with macroalbuminuria due to diabetes’.24
Colour-coded CKD staging table guides management
The primary goals of management are to slow disease progression, preserve kidney function for as long as possible to avoid dialysis or kidney transplant, and reduce absolute cardiovascular risk.21,25
The specific management for each patient is guided by where the patient’s eGFR and ACR results place them on a colour-coded staging table. See Figure 6.
The Kidney Health Australia CKD Management in Primary Care handbook advises that an eGFR < 60 mL/min/1.73 m2 is common in older people, but is nevertheless predictive of significantly increased risks of adverse clinical outcomes, and should not be considered physiological or age appropriate.1
The colour-coded CKD staging table presents the relative risk for developing cardiovascular disease and progression of CKD. The risk levels (low, moderate, high or very high) then correspond to the colour-coded clinical action plans.1,26
They can also be used by health professionals to have a discussion with patients about prognosis when developing an individualised person-centred management plan.
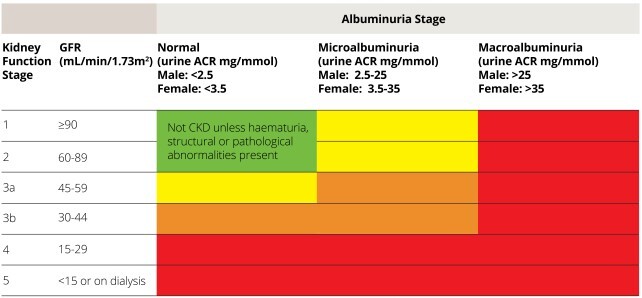
Figure 6: Staging of CKD and colour-coded risk levels that guide clinical action plans for managementa1
a Risk level colour codes; green = low risk, yellow = moderate risk, orange = high risk and red = very high risk.1,26
Source: KHA-CARI Guideline: Early chronic kidney disease: Detection, prevention and management. Johnson DW, Atai E, Chan M, et al. Nephrology 2013;18:340–50. Wiley Online Library.
Read an accessible version of the data in this figure
The green clinical action plan does not require any specific management besides routine follow up in the absence of haematuria, or structural or pathological abnormalities. Yellow includes assessments every 12 months and management for all people with CKD. Orange and red include additional assessments and management. The frequency of review is increased, from every 3–6 months to every 1–3 months, as the risk level increases.1
The majority of people with CKD in the community have mild kidney impairment. Of the one in 10 Australian adults affected by CKD, around 65% have stages 1–2 and less than 10% have stages 4–5.2
Conclusion
Targeted screening and detection of probable CKD can enable GPs to confirm a diagnosis and assess the level of risk of cardiovascular disease and progression of CKD. This in turn guides management. Early detection and subsequent timely management can slow down or even prevent deterioration in kidney function and help to improve cardiovascular outcomes.
NPS MedicineWise CKD program
NPS MedicineWise has developed the Chronic kidney disease: early detection and management program. It is delivering activities and resources for health professionals and consumers including:
- Continuing Professional Development / Educational Visits, including one-to-one visits, small group meetings
- health professional and consumer web content
- consumer resources including patient action plan and fact sheet
- webinar
- podcast
Useful resources
For health professionals
- Kidney Health Australia CKD Management in Primary Care handbook
- RACGP Guidelines for preventive activities in general practice. 9th edition
- RACGP National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people. Chapter 13: Chronic kidney disease prevention and management
- NPS MedicineWise Chronic kidney disease: clinical resources and tools for more guidelines, medicine management strategies and resources
For your patients
- NPS MedicineWise patient resources:
- Card stack: How do I know if my kidneys are healthy and why is it important?
- Factsheet: How healthy are my kidneys and how do I stay well?
- Patient Action Plan: My Kidney Health Plan which can be used with your patients to help them reach their health goals.
- Kidney Health Australia has developed patient resources Books, publications and fact sheets to help manage your patients with kidney disease.
- My Kidneys My Health (handbook) Available as a free hardcopy handbook and as a free mobile smart phone app
- All about chronic kidney disease (fact sheet).
- Make the Link: Chronic Kidney Disease, Diabetes and Cardiovascular Disease (fact sheet).
- This video from Kidney Health Australia explains what your kidneys do and how to keep your kidneys healthy.
- Resources for Aboriginal and Torres Strait Islander peoples.
- Better Health Channel fact sheets
- Kidney Health Australia support services
- Kidney Helpline 1800 454 363 [email protected]
- Kidney Health Australia kidney clubs, buddies and online support groups One-on-one and group peer support programs across Australia.
References
- Kidney Health Australia. Chronic kidney disease (CKD) management in primary care. Melbourne: Kidney Health Australia, 2020 (accessed 5 January 2022).
- Australian Bureau of Statistics. Australian Health Survey: Biomedical Results for Chronic Diseases. Canberra: ABS, 2013 (accessed 9 May 2022).
- Australian Bureau of Statistics. Australian Aboriginal and Torres Strait Islander Health Survey: Biomedical Results, 2012–13. Canberra: ABS, 2014 (accessed 9 May 2022).
- Australian Institute of Health and Welfare. Chronic kidney disease: Australian facts. Canberra: AIHW, 2022. (accessed 16 November 2022).
- Dwyer KD, Robson B, Sum C. How to treat chronic kidney disease. AusDoc How to Treat 2021.
- Chen T, Harris DC. Challenges of chronic kidney disease prevention. Med J Aust 2015;203:209-10.
- Australian and New Zealand Dialysis and Transplant Registry. ANZDATA 44th Annual Report 2020. Adelaide: Australia and New Zealand Dialysis and Transplant Registry, 2020 (accessed 15 May 2022).
- Australian Institute of Health and Welfare. Cardiovascular disease, diabetes and chronic kidney disease - Australian facts: Prevalence and incidence. Cardiovascular, diabetes and chronic kidney disease series no. 2. Canberra: AIHW, 2014 (accessed 15 May 2022).
- Tonelli M, Muntner P, Lloyd A, et al. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: a population-level cohort study. Lancet 2012;380:807-14.
- Australian Bureau of Statistics. Causes of death, Australia, 2017. Canberra: ABS, 2018 (accessed 15 May 2022).
- Tonelli M, Wiebe N, Culleton B, et al. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol 2006;17:2034-47.
- Chu CD, Chen MH, McCulloch CE, et al. Patient Awareness of CKD: A Systematic Review and Meta-analysis of Patient-Oriented Questions and Study Setting. Kidney Med 2021;3:576-85 e1.
- Razavian M, Heeley EL, Perkovic V, et al. Cardiovascular risk management in chronic kidney disease in general practice (the AusHEART study). Nephrol Dial Transplant 2011;27:1396-402.
- Neale EP, Middleton J, Lambert K. Barriers and enablers to detection and management of chronic kidney disease in primary healthcare: a systematic review. BMC Nephrol 2020;21:83.
- White S. Make the Link: Kidneys, Diabetes & Heart. Evidence Report 2021. Melbourne: Kidney Health Australia, 2021 (accessed 10 February 2022).
- Royal Australian College of General Practitioners. Guidelines for preventive activities in general practice. 9th edn. East Melbourne: RACGP, 2016 (accessed 7 June 2022).
- Maple-Brown LJ, Ekinci EI, Hughes JT, et al. Performance of formulas for estimating glomerular filtration rate in Indigenous Australians with and without Type 2 diabetes: the eGFR Study. Diabet Med 2014;31:829-38.
- Johnson DW, Jones GR, Mathew TH, et al. Chronic kidney disease and automatic reporting of estimated glomerular filtration rate: new developments and revised recommendations. Med J Aust 2012;197:224-5.
- Levey AS, de Jong PE, Coresh J, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int 2011;80:17-28.
- Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet 2013;382:339-52.
- Johnson DW, Atai E, Chan M, et al. KHA-CARI guideline: Early chronic kidney disease: detection, prevention and management. Nephrology (Carlton) 2013;18:340-50.
- Khanam MA, Kitsos A, Stankovich J, et al. Chronic kidney disease monitoring in Australian general practice. Aust J Gen Pract 2019;48:132-7.
- Australian Government Department of Health. MBS Health Assessments Items 701, 703, 705 and 707 Canberra: Commonwealth of Australia, 2016 (accessed 16 May 2022).
- Usherwood T, Lee V. Advances in chronic kidney disease pathophysiology and management. Aust J Gen Pract 2021;50:188-92.
- Kalantar-Zadeh K, Jafar TH, Nitsch D, et al. Chronic kidney disease. Lancet 2021;398:786-802.
- Kidney Disease Improving Global Outcomes (KDIGO). Chapter 1: Definition and classification of CKD. Kidney Int Suppl (2011) 2013;3:19-62.